Education for runners and endurance athletes. Learn to train smart, run fast, and be strong.
These articles are free.
Please help keep them alive by buying me a beer:
 Buy me a beer.
Buy me a beer.
This article is part of a series:
→ Part 1 — Hypothermia
→ Part 2 — Risk management
→ Part 3 — Cold acclimation
Also check out my related series on:
Training & racing in the heat.
→ Part 1 — Hypothermia
→ Part 2 — Risk management
→ Part 3 — Cold acclimation
Also check out my related series on:
Training & racing in the heat.
Training & racing in the cold. Part 1 of 3:
Understanding hypothermia.
Thomas Solomon PhD.
First released: 5th Feb 2020.Updated & re-released: 16th Oct 2021.
Winter can be a magical time but it carries some risks. Understanding exercise in cold conditions is critical for maintaining health and fitness development during the winter training phase. Having spent much of my life in cold environments, with this series of articles I intend to shed some light on training smart while successfully avoiding freezing one’s nuts off.
Reading time ~16-mins (3200-words).
Or listen to the Podcast version.
Or listen to the Podcast version.
When Nelly inexplicably instructed everyone in that room to take off all their clothes, one thing was for certain: he was not rapping in a cold climate. During the winter, we must make specific decisions before stepping out the door. Depending on the terrain and the typical climate where you live, you may be able to continue running through the winter but alternative forms of exercise like snowshoeing, hiking, or skiing often become more suitable. Before stepping out the door, some folks choose not to proceed and opt to train indoors for the winter. I once tried that in Cleveland, Ohio, while preparing for an “A” race in the spring armed with nothing but a treadmill and a weights room. The result: all work and no play made this ginger a zero joy boy. I vowed never to do that again and encourage everyone to always plan to train outdoors.
The winter is truly a fun time, even if running is your primary sport. The landscape is beautiful and the conditions are both humbling and educational, allowing you to learn a little more about your physiology and psychology while identifying weaknesses to be remedied in time for the “A” races of your summer season. That said, like Anakin Skywalker, the winter has a dark side - health risks as a consequence of cold exposure. But, learn that it is only fear of the cold that paves the path to the dark side. Overcome any fear, by arming yourself with knowledge.
The first physiological response to cold exposure is vasoconstriction of peripheral blood vessels, which reduces heat transfer from the body core to the surface organs like skin, fat, and muscle to maintain core temperature. But, this comes at the expense of heat loss from your surface organs. This initial process has pronounced effects in the hands and fingers so you experience symptoms like cold and tingling fingers and a loss of manual dexterity. Tying your shoes, opening bags, food, and drinks bottles, and hanging on obstacles all become a problem. You may also notice a decrease in sweat rate, which helps to reduce heat loss from the body, as well as a decrease in heart rate and breathing rate, which helps conserve energy. However, the most obvious sign that cold stress is taking a journey to the dark side is something we have all experienced at some point: shivering.
Cold exposure increases skeletal muscle contractile activity through involuntary shivering or by voluntarily movement or fidgeting. Increased muscle contractions raise metabolic heat production (thermogenesis) to help offset heat loss and maintain thermal balance. Some animals, particularly those that hibernate, can increase metabolic heat production from non-contracting tissue called brown adipose tissue in response to cold exposure. But, in adult humans, brown-fat does not play as large a role in thermogenesis. Shivering is our main defence against heat loss in cold conditions. In cold air, shivering can increase resting whole-body oxygen uptake (VO2) to about 0.6 to 0.7 Litre/min. In cold water, your VO2 can increase beyond 1 L/min at rest. To place this in some meaningful context, consider a well-trained 70 kg athlete who has a resting VO2 of ~0.25 L/min and a VO2max of 4.2 L/min (60 mL/kg/min). During an obstacle course race (OCR), running at around 85% of their VO2max, i.e. ~3570 mL/min, shivering following cold water immersion will dramatically increase VO2 meaning that if this athlete is moving at the same speed, they will be working at a higher relative intensity and will be far less economical (i.e. using far more of their finite fuel supply to move at the same pace). It seems sensible, therefore, that preventing shivering, numb hands, and a loss of manual dexterity is a superb plan. But more on that later…

Freezing one’s nuts off.
Image Copyright © Thomas Solomon. All rights reserved.
In the UK, about 1 in 12 people have asthma. Approximately 80% of people with asthma suffer from exercise-induced bronchoconstriction, a transient narrowing of the airways at the onset of exercise. The signs are a feeling of a tight chest and/or congested airway, with increased frequency in loogie hocking to dislodge respiratory passage mucus. However, exercise-induced bronchoconstriction also affects ~4–20% of healthy people including 11 to 50% of elite athletes. The narrowing of the airways reduces exercise capacity because less oxygen can be consumed (low VO2), less carbon dioxide can be exhaled (low VCO2), and less air can be moved through the lungs in each breath (low tidal volume). Dry air, cold exposure, and even just facial and/or torso cooling are additional triggers for exercise-induced bronchoconstriction. Therefore, the risk of exercise-induced bronchoconstriction is greater in winter, which in many places is characterised by cold and dry conditions.
In people with heart disease, including coronary artery disease (CAD), exercise can cause angina, which is a feeling of squeezing, pressure, heaviness, tightness, or pain in the chest caused by reduced blood flow and oxygen delivery to the heart. Exercising at an intensity below the onset of angina is essential. Exposure to cold, even just facial cooling by wind, increases cardiac muscle oxygen requirements at rest and during exercise while lowering heart rate and increasing peripheral vasoconstriction and mean arterial blood pressure. Therefore, in people with heart disease, cold exposure lowers the exercise intensity at which angina can arise. Furthermore, immersion in water below 25 celsius has been shown to reduce our ability to recognize angina symptoms. This combined with the increased risk of cold-induced bronchoconstriction, which lowers oxygen uptake, means that people with heart disease should be far more vigilant during the winter when selecting exercise intensities. The classic “snow shovelling-induced heart attack” phenomenon also brings attention to strength training. This phenomenon is not specific to snow shovelling but is related to doing unfamiliar exercise that involves isometric muscle contractions (like those that occur during weight lifting) combined with inadvertent breath-holding, causing a rapid and large spike in systolic blood pressure. Not only is choosing aerobic activities below one’s angina threshold recommended for people with heart disease but lifting sensibly with proper technique and breathing is also essential.
Fortunately (or unfortunately, depending on the perspective), I have been dealing with both asthma and coronary artery disease for the past two years and live in the mountains where, in the winter, it is “bollock-freezing” cold. For some first-hand insight, I can personally attest that with careful planning, monitoring, and occasional mission aborting, it is entirely possible to maintain a high level of activity within one’s angina threshold, safely and enjoyably, with minimal cold stress. If you have asthma or heart disease and are concerned about winter exercise, seek medical advice from your GP and/or cardiologist today.

Returning from a mountain run in Banff in -15oC.
Image Copyright © Thomas Solomon. All rights reserved.
Normal body temperature is in the range of 36.5–37.5°C (97.7–99.5°F) and is affected by your age, sex, menstrual cycle, eating, drinking, time of day, and exercise. Hypothermia develops when heat loss exceeds heat production and is defined as a core temperature below 35°C (95°F), which is approximately a 2°C (3.5°F) drop in normal body temperature. However, exercise performance becomes impaired when core temperature drops below 36.8°C (98.2°F; physiological hypothermia).
The symptoms of hypothermia are quite variable from person to person even at the same core temperature, but early symptoms include feeling cold, shivering, and signs of apathy and social withdrawal. More pronounced hypothermia presents like drunkenness with confusion, sleepiness, slurred speech, and a change in behaviour or appearance. Shivering is essential for creating heat because without it there would be a drop in cardiac output (the volume of blood pumped through the heart per minute), blood pressure, breathing rate, and cerebral (brain) blood flow, while cardiac arrhythmia (ventricular fibrillation) becomes detectable. Hypothermia is something to avoid because, if unmanaged, it becomes fatal.
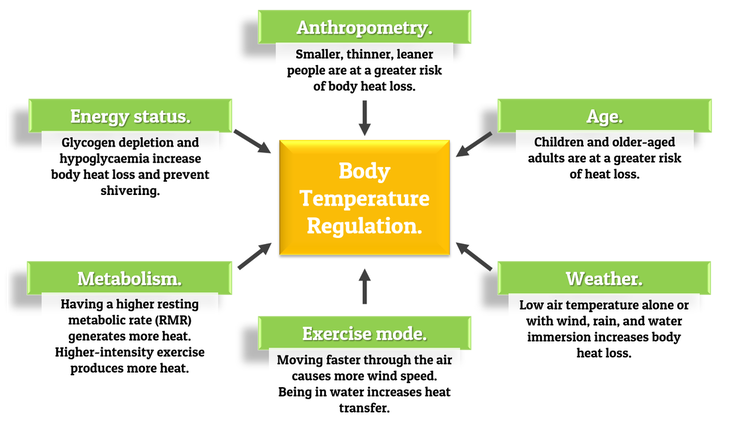
A person can be predisposed to developing hypothermia for a number of reasons. But, in the world of running and obstacle course racing, I have encountered several misunderstandings surrounding the topic. To set things straight, here are some basic facts adapted from the American College of Sports Medicine (ACSM) position stand on the prevention of cold injuries during exercise:
 High physical fitness does not lessen the risk of hypothermia.
High physical fitness does not lessen the risk of hypothermia.
While a fitter person can exercise at a higher intensity for longer and therefore theoretically produce more heat for longer, differences in cold-induced thermoregulation between fitter and less fit individuals are attributable to differences to body size and/or mass rather than a direct effect of fitness. Furthermore, exercise training appears not to alter the thermoregulatory responses to cold exposure. So, if you are highly fit, don’t be flippant.
 Being more muscular and/or festively plump may reduce the risk of hypothermia but does not make you “immune”.
Being more muscular and/or festively plump may reduce the risk of hypothermia but does not make you “immune”.
During exercise, blood flow to muscles increases so skin and fat provide insulation in cold conditions. At rest, however, muscles provide insulative properties so that more muscular people can maintain core temperature better than less muscular folk. People with an excess fat mass also tend to maintain core temperature better than leaner people and have a higher threshold for vasoconstriction, which enables them to better prevent heat loss. Some data show that having a large surface area-to-body-mass ratio causes a more rapid fall in core temperature; however, this difference is not seen between individuals with the same amount of body fat. While anecdotes and some experimental studies have noted sex differences in the response to cold exposure, core temperature responses to cold exposure between men and women are in fact attributable to differences in either body size or levels of fat mass or muscle mass. So, being larger generally helps reduce the risk of hypothermia but being muscular and/or carrying excess fat mass does not make you immune to it.
 Older aged adults and children are at a greater risk of hypothermia.
Older aged adults and children are at a greater risk of hypothermia.
Due to deteriorating vasoconstriction and poorer heat conservation with age, several studies have found that people older than 60-years are less cold-tolerant compared to younger people . Older individuals also appear to have a lower thermal sensitivity to cold, which means they allow air temperatures to fall to lower levels before attempting to warm up. This is particularly dangerous, so go and pay for your grandparents heating bill and glue their thermostat in “on” mode. Children, on the other hand, are also at risk since they typically have a higher body surface area-to-mass ratio and lower levels of fat mass, which allows substantial falls in core temperature when swimming in cold water. So, if you are older-aged (>60 yo) or a child (or coaching such folk), be extra vigilant.
 Wind, rain, and water immersion increases the risk of hypothermia.
Wind, rain, and water immersion increases the risk of hypothermia.
Wind causes exposed objects like skin or clothing to cool down towards the surrounding air temperature more rapidly than without wind. Always take into account wind speed on weather reports but also remembering that such reports do not take into account the wind you produce (note: you do not have to factor in how much fibre you just ate). For example, the additional wind speed to factor in is equal to the speed at which you will be moving through the air. Hence why cycling can feel bloody awful in winter.
If you are headed into the mountains, also always fully evaluate the conditions in your current location as well as the potential conditions where you will head - this not only includes avalanche and/or rock-fall risks but, importantly, also the temperature and exposure. Air temperatures decrease by 2 Celsius for every 310 m (1000 ft) gain in elevation above the site where the air temperature was measured; also, above the tree line, wind speeds are typically higher due to the lack of shelter.
Water can cause considerable body heat loss, even when air temperatures are relatively mild. Since water has a much higher thermal capacity than air, convective heat loss is much greater in rainy weather, in wet clothes, and/or when immersed in water. Although the specific temperature below which individuals are affected can vary greatly between people, the more of a person’s surface area that is exposed to rain or immersed in water, the greater the heat loss is to the water, and the greater the drop in core temperature will be. Studies show that exercise in the rain leads to a more rapid decline in core temperature compared to not exercising.
Although wind and water cause heat loss, your own heat production is also critical. If your exercise intensity is high enough, your body core temperature may be maintained. Exercise at intensities greater than 60% VO2max (i.e. faster than your Easy run pace) can maintain normal core body temperature when the surrounding air temperature is 5°C, clothes are completely wet, and the wind is 5 m/s. However, at light intensities (less than 60% VO2max; i.e. Easy run pace or Hiking etc), body heat loss typically exceeds heat production causing a decline in core temperature. Further work has also found that exercise performed before cold-water immersion also leads to a greater drop in core temperature compared to not exercising, which is quite relevant to the world of OCR. So, if it is windy, raining, and/or you will be getting wet and/or going to higher altitudes, plan, prepare, and be on high alert.
 Depleted energy stores increase the risk of hypothermia.
Depleted energy stores increase the risk of hypothermia.
Food restriction (fasting) for 48-hours prior to exposure to cold water causes core body temperature to decline more rapidly and prevents the onset of shivering, our critical hypothermia-prevention mechanism. But, a 48-hour fast is an extreme scenario and no endurance athlete interested in optimizing their performance should be fasting for such long durations. However, shorter periods without food like an overnight fast followed by high-intensity and/or long-duration exercise can cause hypoglycaemia (a drop in blood glucose below normal levels) which directly impairs the ability to shiver. As such, hypoglycaemia removes your defence against heat loss, increasing the risk of hypothermia. So, in the winter always be extra vigilant with monitoring your food intake to ensure that you are adequately fed, in order to stay safe when exercising in the cold. This is also of great relevance to people with diabetes, so consult your GP or endocrinologist, be informed and stay safe.
Your muscle glycogen levels (your muscles’ store of glucose) are also associated with your response to cold exposure. Glycogen levels change during the night and day and are dictated by the time of day, the amount of carbohydrate you eat, and the intensity and duration of your exercise sessions. Decreased muscle glycogen levels not only lower exercise performance, particularly at higher-intensities (e.g. race pace and beyond), but glycogen depletion also impairs your ability to maintain exercise thermogenesis during cold exposure and blunts initial shivering rates. If you are well-fed, shivering is like a low-intensity exercise in that it relies on fat as the predominant fuel. When blood glucose levels are low (hypoglycaemia), shivering also uses muscle glycogen and an increased number of bursts of shivering depletes greater amounts of muscle glycogen. What does this mean? Well, double trouble. First, less glycogen will lower your power output and speed, thus reducing your exercise performance. Second, with lower power output, you will produce less heat, thus, upon cold exposure, things will quickly turn to the dark side. So, if you plan to exercise in cold and wet/windy conditions, as with all training approaches, become a master of your general and exercise-related nutrition and feed appropriately to prevent hypoglycaemia and top-up your glycogen levels.
Right, that’s all for now. I hope to have provided you with an insight into the physiology of cold exposure to help you to understand the “how” and “why” behind some of the approaches for preventing hypothermia. To summarise the key take-home points related to the factors that influence your core body temperature, please see the Figure below.
In the next part of this series, you will learn more about what to do to train safely in the winter and prevent hypothermia. In the meantime, thanks for reading - be active, stay warm, and keep training smart!
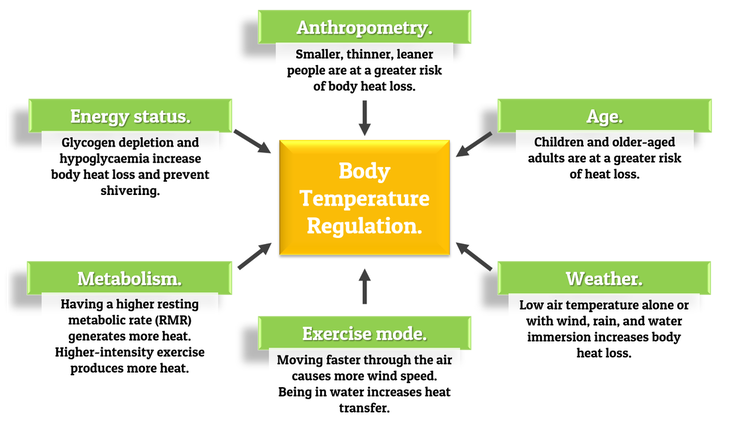
Image Copyright © Thomas Solomon. All rights reserved.
The winter is truly a fun time, even if running is your primary sport. The landscape is beautiful and the conditions are both humbling and educational, allowing you to learn a little more about your physiology and psychology while identifying weaknesses to be remedied in time for the “A” races of your summer season. That said, like Anakin Skywalker, the winter has a dark side - health risks as a consequence of cold exposure. But, learn that it is only fear of the cold that paves the path to the dark side. Overcome any fear, by arming yourself with knowledge.
The physiological effects of cold exposure.
Exposure to cold temperatures removes heat from your body, lowering your peripheral and/or core body temperature. This leads to cold stress, which is characterised by physiological changes in your body that are influenced by the environmental conditions (air temperature, precipitation, altitude, etc) and your own traits (nutritional status, body mass, clothing, etc). Without an effective prevention strategy, cold stress can lead to hypothermia, or cause cold-related injuries like frostbite, trench foot, and chilblains. To help enjoy winter outdoors, it is very important to understand the signs (what you observe) and symptoms (what you experience) of cold stress.The first physiological response to cold exposure is vasoconstriction of peripheral blood vessels, which reduces heat transfer from the body core to the surface organs like skin, fat, and muscle to maintain core temperature. But, this comes at the expense of heat loss from your surface organs. This initial process has pronounced effects in the hands and fingers so you experience symptoms like cold and tingling fingers and a loss of manual dexterity. Tying your shoes, opening bags, food, and drinks bottles, and hanging on obstacles all become a problem. You may also notice a decrease in sweat rate, which helps to reduce heat loss from the body, as well as a decrease in heart rate and breathing rate, which helps conserve energy. However, the most obvious sign that cold stress is taking a journey to the dark side is something we have all experienced at some point: shivering.
Cold exposure increases skeletal muscle contractile activity through involuntary shivering or by voluntarily movement or fidgeting. Increased muscle contractions raise metabolic heat production (thermogenesis) to help offset heat loss and maintain thermal balance. Some animals, particularly those that hibernate, can increase metabolic heat production from non-contracting tissue called brown adipose tissue in response to cold exposure. But, in adult humans, brown-fat does not play as large a role in thermogenesis. Shivering is our main defence against heat loss in cold conditions. In cold air, shivering can increase resting whole-body oxygen uptake (VO2) to about 0.6 to 0.7 Litre/min. In cold water, your VO2 can increase beyond 1 L/min at rest. To place this in some meaningful context, consider a well-trained 70 kg athlete who has a resting VO2 of ~0.25 L/min and a VO2max of 4.2 L/min (60 mL/kg/min). During an obstacle course race (OCR), running at around 85% of their VO2max, i.e. ~3570 mL/min, shivering following cold water immersion will dramatically increase VO2 meaning that if this athlete is moving at the same speed, they will be working at a higher relative intensity and will be far less economical (i.e. using far more of their finite fuel supply to move at the same pace). It seems sensible, therefore, that preventing shivering, numb hands, and a loss of manual dexterity is a superb plan. But more on that later…

Image Copyright © Thomas Solomon. All rights reserved.
×
![]()
Although the above-described physiological responses to cold exposure are normal, people with certain pre-existing clinical conditions are susceptible to a greater risk of cold stress-related morbidity and mortality because the physiological responses can manifest pathophysiological outcomes. This is highly relevant to patients with asthma or coronary artery disease.
In the UK, about 1 in 12 people have asthma. Approximately 80% of people with asthma suffer from exercise-induced bronchoconstriction, a transient narrowing of the airways at the onset of exercise. The signs are a feeling of a tight chest and/or congested airway, with increased frequency in loogie hocking to dislodge respiratory passage mucus. However, exercise-induced bronchoconstriction also affects ~4–20% of healthy people including 11 to 50% of elite athletes. The narrowing of the airways reduces exercise capacity because less oxygen can be consumed (low VO2), less carbon dioxide can be exhaled (low VCO2), and less air can be moved through the lungs in each breath (low tidal volume). Dry air, cold exposure, and even just facial and/or torso cooling are additional triggers for exercise-induced bronchoconstriction. Therefore, the risk of exercise-induced bronchoconstriction is greater in winter, which in many places is characterised by cold and dry conditions.
In people with heart disease, including coronary artery disease (CAD), exercise can cause angina, which is a feeling of squeezing, pressure, heaviness, tightness, or pain in the chest caused by reduced blood flow and oxygen delivery to the heart. Exercising at an intensity below the onset of angina is essential. Exposure to cold, even just facial cooling by wind, increases cardiac muscle oxygen requirements at rest and during exercise while lowering heart rate and increasing peripheral vasoconstriction and mean arterial blood pressure. Therefore, in people with heart disease, cold exposure lowers the exercise intensity at which angina can arise. Furthermore, immersion in water below 25 celsius has been shown to reduce our ability to recognize angina symptoms. This combined with the increased risk of cold-induced bronchoconstriction, which lowers oxygen uptake, means that people with heart disease should be far more vigilant during the winter when selecting exercise intensities. The classic “snow shovelling-induced heart attack” phenomenon also brings attention to strength training. This phenomenon is not specific to snow shovelling but is related to doing unfamiliar exercise that involves isometric muscle contractions (like those that occur during weight lifting) combined with inadvertent breath-holding, causing a rapid and large spike in systolic blood pressure. Not only is choosing aerobic activities below one’s angina threshold recommended for people with heart disease but lifting sensibly with proper technique and breathing is also essential.
Fortunately (or unfortunately, depending on the perspective), I have been dealing with both asthma and coronary artery disease for the past two years and live in the mountains where, in the winter, it is “bollock-freezing” cold. For some first-hand insight, I can personally attest that with careful planning, monitoring, and occasional mission aborting, it is entirely possible to maintain a high level of activity within one’s angina threshold, safely and enjoyably, with minimal cold stress. If you have asthma or heart disease and are concerned about winter exercise, seek medical advice from your GP and/or cardiologist today.

Image Copyright © Thomas Solomon. All rights reserved.
×
![]()
Hypothermia.
When training and/or racing in cold conditions, the major consideration is maintaining body temperature. Most runners will have experienced the signs and symptoms of cold exposure. Obstacle racers are undoubtedly at greater risk since they are regularly exposed to cold air with cold water immersion and heavy lifting in all weather conditions. Don’t be a hero, hypothermia is serious.Normal body temperature is in the range of 36.5–37.5°C (97.7–99.5°F) and is affected by your age, sex, menstrual cycle, eating, drinking, time of day, and exercise. Hypothermia develops when heat loss exceeds heat production and is defined as a core temperature below 35°C (95°F), which is approximately a 2°C (3.5°F) drop in normal body temperature. However, exercise performance becomes impaired when core temperature drops below 36.8°C (98.2°F; physiological hypothermia).
The symptoms of hypothermia are quite variable from person to person even at the same core temperature, but early symptoms include feeling cold, shivering, and signs of apathy and social withdrawal. More pronounced hypothermia presents like drunkenness with confusion, sleepiness, slurred speech, and a change in behaviour or appearance. Shivering is essential for creating heat because without it there would be a drop in cardiac output (the volume of blood pumped through the heart per minute), blood pressure, breathing rate, and cerebral (brain) blood flow, while cardiac arrhythmia (ventricular fibrillation) becomes detectable. Hypothermia is something to avoid because, if unmanaged, it becomes fatal.
A person can be predisposed to developing hypothermia for a number of reasons. But, in the world of running and obstacle course racing, I have encountered several misunderstandings surrounding the topic. To set things straight, here are some basic facts adapted from the American College of Sports Medicine (ACSM) position stand on the prevention of cold injuries during exercise:
While a fitter person can exercise at a higher intensity for longer and therefore theoretically produce more heat for longer, differences in cold-induced thermoregulation between fitter and less fit individuals are attributable to differences to body size and/or mass rather than a direct effect of fitness. Furthermore, exercise training appears not to alter the thermoregulatory responses to cold exposure. So, if you are highly fit, don’t be flippant.
During exercise, blood flow to muscles increases so skin and fat provide insulation in cold conditions. At rest, however, muscles provide insulative properties so that more muscular people can maintain core temperature better than less muscular folk. People with an excess fat mass also tend to maintain core temperature better than leaner people and have a higher threshold for vasoconstriction, which enables them to better prevent heat loss. Some data show that having a large surface area-to-body-mass ratio causes a more rapid fall in core temperature; however, this difference is not seen between individuals with the same amount of body fat. While anecdotes and some experimental studies have noted sex differences in the response to cold exposure, core temperature responses to cold exposure between men and women are in fact attributable to differences in either body size or levels of fat mass or muscle mass. So, being larger generally helps reduce the risk of hypothermia but being muscular and/or carrying excess fat mass does not make you immune to it.
Due to deteriorating vasoconstriction and poorer heat conservation with age, several studies have found that people older than 60-years are less cold-tolerant compared to younger people . Older individuals also appear to have a lower thermal sensitivity to cold, which means they allow air temperatures to fall to lower levels before attempting to warm up. This is particularly dangerous, so go and pay for your grandparents heating bill and glue their thermostat in “on” mode. Children, on the other hand, are also at risk since they typically have a higher body surface area-to-mass ratio and lower levels of fat mass, which allows substantial falls in core temperature when swimming in cold water. So, if you are older-aged (>60 yo) or a child (or coaching such folk), be extra vigilant.
Wind causes exposed objects like skin or clothing to cool down towards the surrounding air temperature more rapidly than without wind. Always take into account wind speed on weather reports but also remembering that such reports do not take into account the wind you produce (note: you do not have to factor in how much fibre you just ate). For example, the additional wind speed to factor in is equal to the speed at which you will be moving through the air. Hence why cycling can feel bloody awful in winter.
If you are headed into the mountains, also always fully evaluate the conditions in your current location as well as the potential conditions where you will head - this not only includes avalanche and/or rock-fall risks but, importantly, also the temperature and exposure. Air temperatures decrease by 2 Celsius for every 310 m (1000 ft) gain in elevation above the site where the air temperature was measured; also, above the tree line, wind speeds are typically higher due to the lack of shelter.
Water can cause considerable body heat loss, even when air temperatures are relatively mild. Since water has a much higher thermal capacity than air, convective heat loss is much greater in rainy weather, in wet clothes, and/or when immersed in water. Although the specific temperature below which individuals are affected can vary greatly between people, the more of a person’s surface area that is exposed to rain or immersed in water, the greater the heat loss is to the water, and the greater the drop in core temperature will be. Studies show that exercise in the rain leads to a more rapid decline in core temperature compared to not exercising.
Although wind and water cause heat loss, your own heat production is also critical. If your exercise intensity is high enough, your body core temperature may be maintained. Exercise at intensities greater than 60% VO2max (i.e. faster than your Easy run pace) can maintain normal core body temperature when the surrounding air temperature is 5°C, clothes are completely wet, and the wind is 5 m/s. However, at light intensities (less than 60% VO2max; i.e. Easy run pace or Hiking etc), body heat loss typically exceeds heat production causing a decline in core temperature. Further work has also found that exercise performed before cold-water immersion also leads to a greater drop in core temperature compared to not exercising, which is quite relevant to the world of OCR. So, if it is windy, raining, and/or you will be getting wet and/or going to higher altitudes, plan, prepare, and be on high alert.
Food restriction (fasting) for 48-hours prior to exposure to cold water causes core body temperature to decline more rapidly and prevents the onset of shivering, our critical hypothermia-prevention mechanism. But, a 48-hour fast is an extreme scenario and no endurance athlete interested in optimizing their performance should be fasting for such long durations. However, shorter periods without food like an overnight fast followed by high-intensity and/or long-duration exercise can cause hypoglycaemia (a drop in blood glucose below normal levels) which directly impairs the ability to shiver. As such, hypoglycaemia removes your defence against heat loss, increasing the risk of hypothermia. So, in the winter always be extra vigilant with monitoring your food intake to ensure that you are adequately fed, in order to stay safe when exercising in the cold. This is also of great relevance to people with diabetes, so consult your GP or endocrinologist, be informed and stay safe.
Your muscle glycogen levels (your muscles’ store of glucose) are also associated with your response to cold exposure. Glycogen levels change during the night and day and are dictated by the time of day, the amount of carbohydrate you eat, and the intensity and duration of your exercise sessions. Decreased muscle glycogen levels not only lower exercise performance, particularly at higher-intensities (e.g. race pace and beyond), but glycogen depletion also impairs your ability to maintain exercise thermogenesis during cold exposure and blunts initial shivering rates. If you are well-fed, shivering is like a low-intensity exercise in that it relies on fat as the predominant fuel. When blood glucose levels are low (hypoglycaemia), shivering also uses muscle glycogen and an increased number of bursts of shivering depletes greater amounts of muscle glycogen. What does this mean? Well, double trouble. First, less glycogen will lower your power output and speed, thus reducing your exercise performance. Second, with lower power output, you will produce less heat, thus, upon cold exposure, things will quickly turn to the dark side. So, if you plan to exercise in cold and wet/windy conditions, as with all training approaches, become a master of your general and exercise-related nutrition and feed appropriately to prevent hypoglycaemia and top-up your glycogen levels.
In the next part of this series, you will learn more about what to do to train safely in the winter and prevent hypothermia. In the meantime, thanks for reading - be active, stay warm, and keep training smart!
×
![]()
Disclaimer: I occasionally mention brands and products but it is important to know that I am not affiliated with, sponsored by, an ambassador for, or receiving advertisement royalties from any brands. I have conducted biomedical research for which I have received research money from publicly-funded national research councils and medical charities, and also from private companies, including Novo Nordisk Foundation, AstraZeneca, Amylin, A.P. Møller Foundation, and Augustinus Foundation. I’ve also consulted for Boost Treadmills and Gu Energy on their research and innovation grant applications and I’ve provided research and science writing services for Examine — some of my articles contain links to information provided by Examine but I do not receive any royalties or bonuses from those links. These companies had no control over the research design, data analysis, or publication outcomes of my work. Any recommendations I make are, and always will be, based on my own views and opinions shaped by the evidence available. My recommendations have never and will never be influenced by affiliations, sponsorships, advertisement royalties, etc. The information I provide is not medical advice. Before making any changes to your habits of daily living based on any information I provide, always ensure it is safe for you to do so and consult your doctor if you are unsure.
If you find value in this free content, please help keep it alive and buy me a beer:
 Buy me a beer.
Buy me a beer.
Share this post on your social media:
Want free exercise science education delivered to your inbox? Join the 100s of other athletes, coaches, students, scientists, & clinicians and sign up here:

About the author:
I am Thomas Solomon and I'm passionate about relaying accurate and clear scientific information to the masses to help folks meet their fitness and performance goals. I hold a BSc in Biochemistry and a PhD in Exercise Science and am an ACSM-certified Exercise Physiologist and Personal Trainer, a VDOT-certified Distance running coach, and a Registered Nutritionist. Since 2002, I have conducted biomedical research in exercise and nutrition and have taught and led university courses in exercise physiology, nutrition, biochemistry, and molecular medicine. My work is published in over 80 peer-reviewed medical journal publications and I have delivered more than 50 conference presentations & invited talks at universities and medical societies. I have coached and provided training plans for truck-loads of athletes, have competed at a high level in running, cycling, and obstacle course racing, and continue to run, ride, ski, hike, lift, and climb as much as my ageing body will allow. To stay on top of scientific developments, I consult for scientists, participate in journal clubs, peer-review papers for medical journals, and I invest every Friday in reading what new delights have spawned onto PubMed. In my spare time, I hunt for phenomenal mountain views to capture through the lens, boulder problems to solve, and for new craft beers to drink with the goal of sending my gustatory system into a hullabaloo.
Copyright © Thomas Solomon. All rights reserved.
I am Thomas Solomon and I'm passionate about relaying accurate and clear scientific information to the masses to help folks meet their fitness and performance goals. I hold a BSc in Biochemistry and a PhD in Exercise Science and am an ACSM-certified Exercise Physiologist and Personal Trainer, a VDOT-certified Distance running coach, and a Registered Nutritionist. Since 2002, I have conducted biomedical research in exercise and nutrition and have taught and led university courses in exercise physiology, nutrition, biochemistry, and molecular medicine. My work is published in over 80 peer-reviewed medical journal publications and I have delivered more than 50 conference presentations & invited talks at universities and medical societies. I have coached and provided training plans for truck-loads of athletes, have competed at a high level in running, cycling, and obstacle course racing, and continue to run, ride, ski, hike, lift, and climb as much as my ageing body will allow. To stay on top of scientific developments, I consult for scientists, participate in journal clubs, peer-review papers for medical journals, and I invest every Friday in reading what new delights have spawned onto PubMed. In my spare time, I hunt for phenomenal mountain views to capture through the lens, boulder problems to solve, and for new craft beers to drink with the goal of sending my gustatory system into a hullabaloo.
Copyright © Thomas Solomon. All rights reserved.
