OPINION:
Continuous glucose monitoring for athletes. The “glucose performance zone” is all hype.
Thomas Solomon PhD.
27th Nov 2021.
CGM, aka Continuous Glucose Monitoring, is a tool used in diabetes treatment (read about that here and here) that is now being marketed to athletes to teach them to adequately fuel their sessions and races. But, is CGM for athletes a new age fueling tool or just another fad? Read on to hear my opinion… But, first let me explain why I have the right to an opinion on this topic…
Between 2009 and 2018, I used CGM devices in several clinical studies including ~150 subjects (see my CGM publications here). I started with Medtronic’s CGMS System Gold moving on to Medtronic’s Guardian and iPro2 models, and eventually transitioning to Dexcom’s G5 and G6 models. I have also worn all those models in pilot testing for said studies. More recently and more relevantly, I have used Abbott’s Libre Sense Glucose Sport Biosensor (the CGM being used by Supersapiens). Furthermore, I spent my entire academic career studying human metabolism, nutrition, and exercise physiology, with a specific focus on glucose metabolism and blood glucose control — I have over 80 publications on this topic. I am also a coach. And, although I no longer consider myself an athlete, I continue to train and occasionally race. The bottom line... I am very familiar with CGM technology, have witnessed its development, understand its limitations, have a deep understanding of glucose metabolism and how it applies to training as a practitioner and a doer; and, most importantly, am not sponsored by, affiliated with, or receiving royalties from either Abbot, Dexcom, or Medtronic. Forever and ever, Amen.
Right with that out the way…
Persistently high blood glucose is undesirable because constantly exposing your organs to excessively high glucose triggers molecular events that massively increase the risk of a whole host of undesirables — stroke, heart attack, dementia, retinal failure, kidney failure, nerve failure, and so on…
Reducing persistently-elevated blood glucose levels in folks with diabetes drastically reduces their risk and improves their quality of life. People with diabetes — including athletes with diabetes — achieve this by managing their blood glucose with diet, exercise, and a menu of glucose-lowering drugs, including insulin.
Sweet.
CGM can help people with diabetes monitor blood glucose to help optimize their feeding, activity, and insulin dosages. Therefore, CGM can help folks learn to manage their diabetes while providing doctors with prognostic information. Sounds amazing. But, with any tool, it is always important to understand what the data tells you and what its limitations are. So...
And
High glucose exposure and high glucose variability are each predictive of increased risk of “undesirable shiz”. But, while CGM data analysis is simple, CGM data interpretation is not. This brings me to...
Progress!
But, there are some limitations...
Firstly, due to the uncertain cost-effectiveness economics — i.e. simply having a CGM does not make a person’s diabetes disappear — healthcare systems do not dish CGMs out to all patients. Typically only folks who can afford it or those who can afford health insurance that covers it, get their mitts on a CGM. For example, the Medtronic iPro2 is ~€250 every 4-weeks (4 × 1-week sensors) plus ~€1200 upfront for the transmitter unit (which lasts forever) while the Dexcom G5/G6 is ~€250 for 4-weeks (4 × 1-week sensors) plus ~€250 every 3-months for the transmitter unit.
Secondly, to measure the concentration of glucose (or any metabolite) circulating in the blood (or, more accurately, the blood plasma, the “water” fraction of blood in which metabolites are dissolved, or even more accurately, the interstitial fluid between the blood and your tissues, in the case of CGM), we need three things:
 A measurement tool (a biochemical assay) that is accurate — hits the true value every time — and precise — hits the same number every time.
A measurement tool (a biochemical assay) that is accurate — hits the true value every time — and precise — hits the same number every time.
 The amount of glucose in the blood needs to be relatively constant.
The amount of glucose in the blood needs to be relatively constant.
And/or
 The amount of plasma (i.e. water in which glucose is dissolved in) also needs to be relatively constant.
The amount of plasma (i.e. water in which glucose is dissolved in) also needs to be relatively constant.
The biochemical assays used in CGM have been optimised since ~1960 and are highly accurate and precise. But, they are also influenced by several things… Excessive vitamin C intake can ruin the accuracy of a glucose dehydrogenase assay while the presence of paracetamol (acetaminophen) or hypoxia (low blood oxygen that can occur at high altitude or during prolonged high-intensity exercise) can ruin the accuracy of a glucose oxidase assay. Although the amount of glucose in the blood frequently changes throughout the day, CGM minimises the magnitude of these fluctuations by measuring glucose very frequently (every ~5 to 15-mins). However, plasma volume shifts also occur during the day and these are hard to control. That said, when you are not exercising, changes in plasma volume are relatively small and slow to occur. Therefore, at rest, CGM has acceptably high accuracy, described as MARD (or mean absolute relative difference) in clinical trials (go deep on MARD here and here).
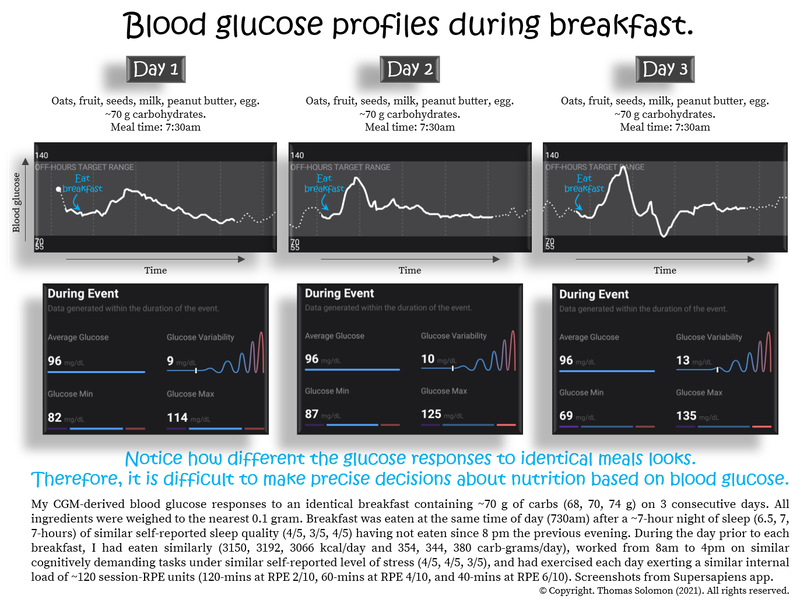
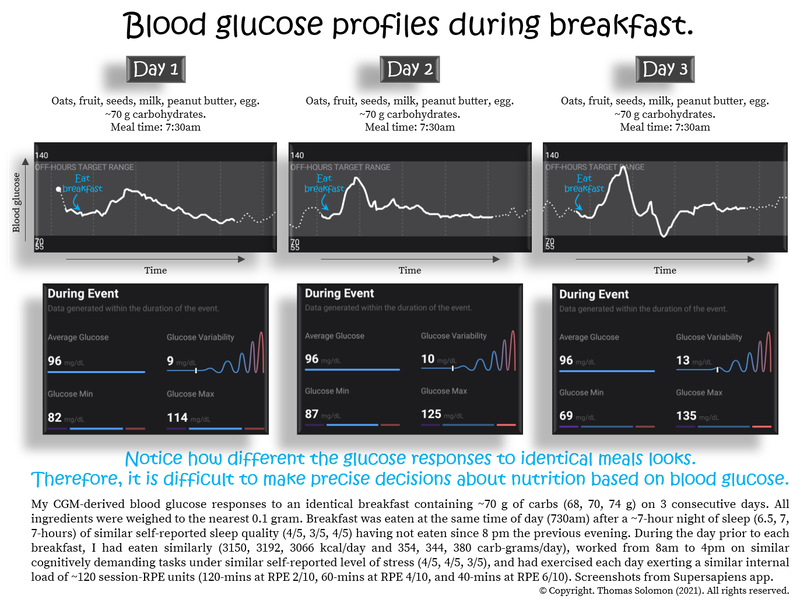
Thirdly, while CGM accuracy (or MARD) is acceptable, its precision is questionable… Initially, evidence supported CGM in helping people establish “personalised nutrition” (see here, here, and here). But, when different meals are ranked according to their blood glucose response, the within-person variability of glucose responses to the same meals is huge. Furthermore, CGM devices from different companies rank meals in a very different order. This means that the error of measurement of CGM as a biomarker for blood glucose is rather large and is not just caused by consistent error (bias) but also variable error (aka noise). Such poor precision may lead to imprecise nutritional decisions.
And, lastly, if you have ever worn and/or seen data generated by a CGM, you will know that the data is not smooth eye-pleasing curves of glucose climbing and falling — biology is erratic. Meal-to-meal glucose responses are not consistent and you have to be careful to avoid “availability heuristics” that bias your interpretation and make you believe that “what you see is all there is”. For example, if you just ate white bread and glucose goes up, this does not mean that you should never eat white bread. Furthermore, if you ate white bread today and the response was smaller than it was yesterday does not mean that you are healthier today. Consequently, the major limitation of CGM is that to interpret CGM data and respond to it appropriately, you need knowledge of nutrient metabolism and behavioural psychology.
Now is a good time to mention that, in the clinical world of diabetes, using CGM for assessing blood glucose during exercise is an area of debate...
The first thing to note is the time lag between changes in blood glucose (which is what your body is exposed to) and interstitial glucose (which is what CGM measures). The current evidence shows that CGM accuracy (or MARD) during higher intensity exercise is poorest during the earlier stages of a bout, even in the newest models. But, this does not imply that CGM is bad but it is important for people with diabetes because if CGM glucose is low during exercise it means their actual blood glucose is likely lower. Consequently, patients who suspect hypoglycemia during exercise are advised to confirm glucose with an accurate and precise finger prick measurement rather than relying on what the CGM is telling them.
Some studies show that CGM accuracy is reasonable during low-intensity walking (on average, MARD is ~17% when a 30-min walk starts after a meal and ~19% when walking before eating, using a FreeStyle Libre device). But during more vigorous exercise, MARD values for FreeStyle Libre start to inflate. For example, in one study, on average, MARD was ~30% during 45-minutes of moderate-intensity exercise.
To help put these values in context, a MARD value of 30% means that the CGM-measured value is 30% higher than the current blood glucose value, i.e. when blood glucose is truly 100 mg/dL (~5.6 mmol/L), the CGM gives a value of 130 mg/dL (or ~7.3 mmol/L). This can be a problem for people with diabetes because hypoglycemic blood glucose values below 70 mg/dL (~4 mmol/L) during exercise, would be indicated as “within the healthy range” on the CGM.
Other brands have been found to perform a little better. For example, the Dexcom G6 has shown slightly better and more consistent accuracy during fixed-intensity aerobic (MARD: 8.9 to 13.9%), interval (12.1 to 16.8%), and resistance (7.7 to 14.5%) exercise bouts. But, in 2021, Da Prato and colleagues evaluated several devices simultaneously, finding that CGM accuracy during exercise was generally poor for all devices, MARD ranging from 16% to 28% to 30% to 45%, depending on devices and types of exercise.
But perhaps I am cherry-picking studies?
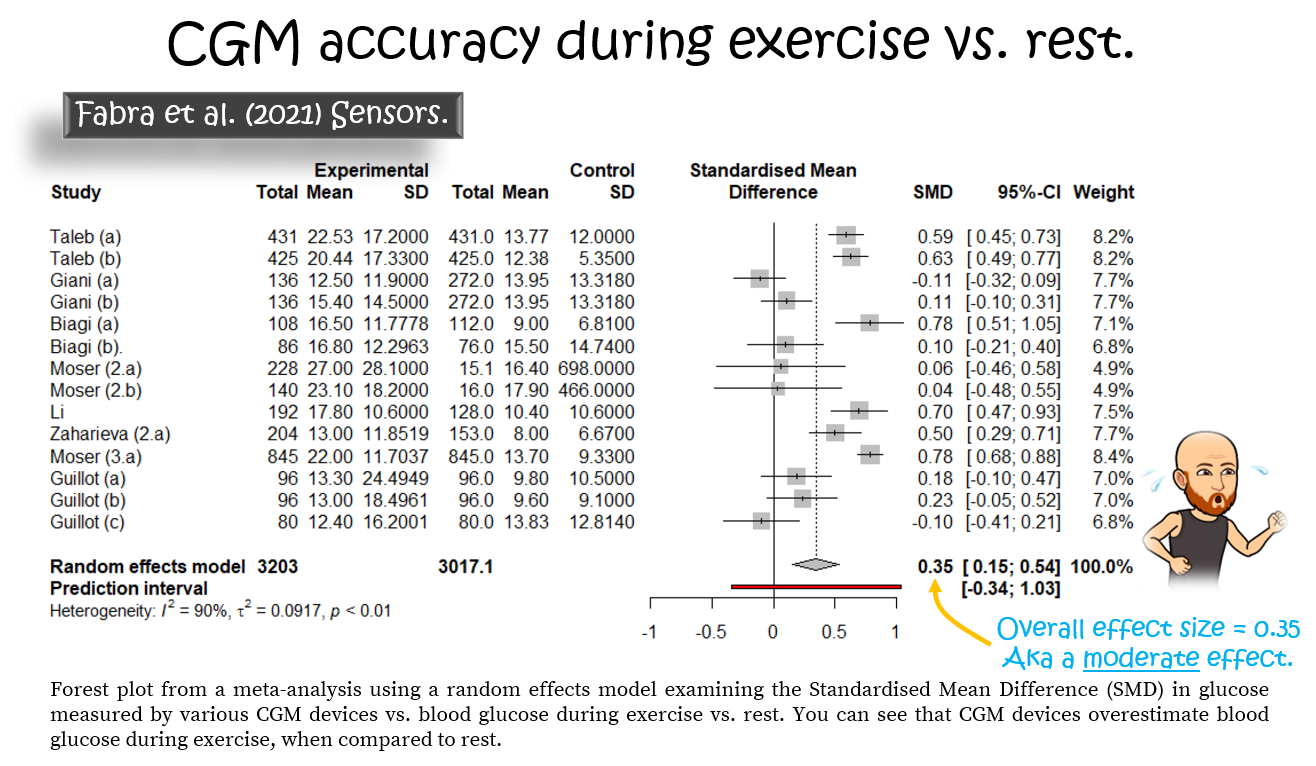
Fear not… In 2021, Fabra et al. systematically reviewed the evidence for several Medtronic, Dexcom, and Abbot devices. Their meta-analysis showed massive variability between devices and that CGM devices overestimate blood glucose during exercise compared to rest with a moderate effect size of 0.35. They concluded that “the more recent sensor used, the better the technology and more accurate the CGM devices are”, which is encouraging.

They aim to revolutionise fuelling in sport using a “Glucose Performance Zone” concept, claiming that real-time blood glucose measurements act as a “fuel gauge” and claiming that high blood glucose equals lots of fuel in the tank, which equals you will go faster. Their marketing is slick and the idea sounds pretty punchy. Investors certainly thought so — initial capital searching raised $13.5 million! Plus, they are using the very clever “Maurten marketing model” of using big investment income to sponsor as many big names in endurance sport as they can to endorse their product. For example, Supersapiens is the new title sponsor of Ironman World Champs in Hawaii and have sponsorship-contracts with pro cycling teams, Ineos Grenadiers and Jumbo Visma, the great Eliud Kipchoge and hundreds (!) of other athletes.
It is very impressive. But, you’ve probably guessed that I am not mesmerized by their narrative (and nor were the UCI who, in 2021, banned the use of CGM during cycling races, partially upholding their “no needle” policy).
Why the negative mood, Solomon?
Well, to start, their “Glucose Performance Zone” and “fuel gauge” concepts are not supported by any evidence. This might sound surprising since Supersapiens has published several blog articles highlighting the “evidence” (for examples, see “The Close Ties Between Glucose Levels and Athletic Performance” and “Go Faster Longer: Use CGM To Know What Glucose Levels You Should Maintain To Maximise Your Training” and “Glucose Zones: Where To Manage Your Glucose Levels To Reduce Inflammation And Promote Recovery”). But, their home page and “education hub” blog pages don’t cite any actual evidence. Yes, these pages look impressive with lists of citations but the act of listing scientific papers is not a goldpass for supporting evidence.
When you scratch beneath the surface, Supersapiens have simply used an approach that many students have tried to slip under my radar in their assignments — they refer to papers that merely mention the topic in question rather than papers that test relevant hypotheses and generate relevant data. I will get to the actual evidence in a moment, but the “scientific theory” they have compiled is shoddy and the narratives are written simply to fit the goal of the product. That is, after all, how many companies sell us new products. But, if they were a student in my class, they’d get a D-grade and some notes on how to use published evidence.
Beyond that, I also fear Supersapiens are promoting unhealthy eating practices. One of their recent blog posts (“Fresh Take On Fuelling”) says: “A bowl of gels for breakfast is not conventionally accepted as a good start to the day, yet we seem to find this ideal when exercising in the morning.”. As an academic, coach, former athlete, and human who cares about people’s performance AND health, this truly gets me tugging at my ginger beard. No athlete should swap healthy whole foods for gels at any meal, ever. I suspect there is probably a Supersapiens-Maurten collaboration on the horizon… Anyway, enough about that...
Blood glucose is constantly being sipped up by your brain, muscles, fat tissue, and other organs to produce energy. But blood glucose levels are maintained within a tight range and your liver does a phenomenal job of producing (gluconeogenesis) and releasing glucose (glycogen breakdown) back into the blood to prevent hypoglycemia — low blood sugar — which would kill you if not stopped.
During exercise, your muscles start gobbling large amounts of glucose from the blood to maintain energy production. If your body did nothing about this, hypoglycemia would occur in minutes. But your liver is awesome and responds preemptively to keep you rocking...
One fundamental aspect of human physiology Supersapiens have overlooked is the effect of “stress” on liver glucose output. In this context, exercise — a physical stress — increases adrenaline release, causing a glucagon response that increases glucose output from your liver. This is part of your fight or flight response that helped your ancestors successfully deliver you to your place on Earth. In fact, one of the key life-saving tools for a type 1 diabetic athlete who is plunging into hypoglycemia during exercise when they don’t have food available is to do some sprints. Why? Because the high intensity triggers adrenaline release and a subsequent rapid release of glucose from the liver into the blood. But this doesn’t only occur in diabetic patients. This fundamental biology occurs in all of us.
What is my point?
Well, if you go do anything with intermittent bursts of high intensity and you are wearing a CGM, you will see that your blood glucose will rise as you start your warm-up and probably spike intermittently as you unleash your mayhem. This is fundamental biology that was discovered long before I was delivered to Earth 41 years ago.
During interval sessions and weights sessions AND during prolonged hard races, your “fuel tank” (aka glycogen) is continuously depleted. Stored glycogen in your muscles and your liver slowly decrease but blood glucose does not. In fact, during a prolonged high-intensity race you will see your blood glucose rise and remain above baseline concentrations.

Blood glucose is not a biomarker for glycogen except perhaps when glycogen levels are depleted and blood glucose is the only food your muscles have to keep on rocking. For this reason, blood glucose during exercise tells you nothing about your “fuel tank” nor, therefore, can it be a “fuel gauge”. So, what will continuous blood glucose readings during exercise tell you about performance?
Not much.
But, that is just my narrative. An important question is...
But how do CGMs fit into this story?
Back in May, I ran a self-supported 60 km loop in my local mountains with ~2000 metres of elevation gain and loss. I ate 353 kcals per hour, including 76 grams of carbs per hour, and with Abbott’s Libre Sense Glucose Sport Biosensor — Supersapiens — I collected CGM data throughout but blinded myself to the data and, therefore, it did not inform my feeding choices. My average glucose was 134 mg/dL with a glucose variability (standard deviation) of 9 mg/dL and a range of 110 to 161 mg/dL. Since it's not possible to download the raw Supersapiens data, I could only visually compare my blood glucose concentrations with my grade-adjusted pace during the run — there was no apparent relationship.
But that is just a bias-filled anecdote from personal use. What about objective studies?
In 2015, Sengoku and colleagues used Medtronic’s System Gold CGM to observe blood glucose in 2 ultrarunners during a 100 km race. During the race, blood glucose gradually increased but, while the faster of the two racers maintained their blood glucose throughout the race, the slower runner had a sharp drop in their blood glucose eventually resulting in hypoglycemia (less than 70 mg/dL or ~4 mmol/L), despite similar during-race feeding habits.
In 2020, Kengo Ishihara and colleagues published a similar observational study using Abbott’s FreeStyle Libre CGM to monitor blood glucose in 4 male and 3 female ultrarunners during a 160 km mountain race. By the end of the race, runners’ average glucose concentration rose from ~104 to ~164 mg/dL (~5.8 to ~9.1 mmol/L) and the total amount of carbohydrate intake during the race ranged from 16.3 to 52.9 g/h. Runners did not use the CGM to inform their feeding decisions but a greater carbohydrate intake positively correlated with faster running speeds (R2=0.80 and P=0.007, which means that 80% of the variance in speed was explained by the amount of carb intake and that there is a measly 0.7% chance that this strong association is due to random chance) and those with higher carb intake better maintained their blood glucose during the race.
But, was blood glucose correlated with race speed?
Yes, but with nuances...
Rather than simply comparing the average (mean) blood glucose and the spread (standard deviation) of values with running speed, they compared the change in glucose (end of race minus baseline) vs. speed and then stratified the changes into arbitrary “lowest”, “average”, and “largest” changes (without defining what lowest, average, and largest mean). This is an odd “data mining” analysis, especially when you only have 7 subjects, because it screams, “we were fishing to find significance”. Anyway, they found that the “lowest” (males: R2=0.24, P=0.003; females: R2=0.14, P=0.05) and “average” (males: R2=0.17, P = 0.02; females: R2=0.05, P = 0.24) glucose changes were positively related to faster speeds but that the “largest” change in glucose was not (males: R2=0.0005, P=0.90; females: R2=0.01, P=0.57). Yikes, that is confusing.
In 2021, another observational study of 1 female athlete racing a 438 km FKT around Lake Biwa was published in 2021 by the same group. Using Abbot’s Freestyle Libre, they found that her average daytime and nighttime blood glucose were ~130 and ~125 mg/dL. By dividing the distance into 32 segments, the authors found that her running speed was associated with total energy (P=0.02) and carbohydrate intake (P=0.01), specifically for solid foods vs. liquids and gels, but that her blood glucose concentrations did not correlate with running speeds.
Why do Supersapiens not cite them?
Perhaps because the studies do not support their “glucose performance zone” or “fuel gauge” narratives. Instead, these studies simply use real-world and meaningful race day conditions to confirm what we already knew:
 Carbohydrate intake during prolonged duration races is associated with better performance.
Carbohydrate intake during prolonged duration races is associated with better performance.
But…
 We don’t need a CGM to tell us that.
We don’t need a CGM to tell us that.
And…
 The data from a CGM is unable to tell us that.
The data from a CGM is unable to tell us that.
So, the final important question to ask...
I previously went deep on this topic at veohtu.com/thefuelinyourbody, veohtu.com/burningfuelduringexercise, and veohtu.com/howlongcanyougo. But, to summarise that info, the fuel available to you during exercise can be conceptualised as:
 A bucket load of fatty acids and a pint-glass of glucose.
A bucket load of fatty acids and a pint-glass of glucose.
To put numbers on this, a 65 kg person with 15% body fat has ~10,000 grams of fat and a mere ~500 grams of glucose most of which is stored in muscle (~400 g) and liver (~100 g) glycogen with a little (~4 g) floating around in the blood. (Note that glycogen stores are greatest in endurance athletes eating a high carb diet and lowest in keto-eaters and to see how that affects exercise metabolism, check out my Performance Nutrition series). During exercise, your muscles “burn” glucose (from glycogen and from the blood) at increasingly higher rates as exercise intensity increases while your liver breaks down glycogen to throw glucose back into the blood to prevent blood glucose falling. Since the rate of glucose “burning” can reach ~5 grams per minute during prolonged hard work, stored glycogen only lasts for ~1½ to 2-hours. But, during that time, blood glucose doesn’t gradually drop; it remains constant and only drops when liver glycogen has been gobbled up.
My point is that your blood is simply a “vessel” in which glucose is transported between tissues. Despite the importance of glucose as the major fuel for hard work,
 Blood glucose is not a fuel gauge, tissue glycogen (and fat) levels are.
Blood glucose is not a fuel gauge, tissue glycogen (and fat) levels are.
And,
 High blood glucose concentrations do not represent high glycogen stores.
High blood glucose concentrations do not represent high glycogen stores.
And,
 Low blood glucose concentrations do not represent low glycogen stores EXCEPT when glycogen stores are critically low.
Low blood glucose concentrations do not represent low glycogen stores EXCEPT when glycogen stores are critically low.
This means that Supersapiens alleged “Glucose Performance Zone” of 110 to 180 mg/dL is not evidence-informed but completely fabricated. It also means that a drop in your blood glucose within this imaginary “zone”, say from 180 to 170, or 150 to 140, or 120 to 110 mg/dL, does not mean that your fuel stores are lower and, therefore, does not trigger feelings of fatigue and does not make you slow down. A drop in blood glucose concentration simply means that, at that time, more glucose has left the blood than has entered the blood.
That said, when your blood glucose approaches hypoglycemic levels and drops below ~70 mg/dL (~4 mmol/L), a different story emerges. Hypoglycemia can hint that accessible fuel is low — during exercise, hypoglycemia typically indicates that your liver glycogen is low and/or you have exceeded your liver’s capacity to produce “new” glucose. And, now you're in trouble because if blood glucose keeps falling, fatigue signals will be sent to your brain and you will very likely succumb to Darth Fader (the Sith Lord of fatigue) and slow down.
When Supersapiens write enticing statements like “Average Glucose is naturally regulated around 90-110 mg/dL, but may need to be higher for you leading into a training or performance event”, they are just using the power of suggestion. There is no evidence that you need to raise your fasting glucose level above baseline to increase performance. If we have learned anything about fueling during exercise over the last 100-years it is that we do not and should not wait for blood glucose to change to consider a fueling choice. When blood glucose drops too low, you will be in trouble. Plus, what we currently know about CGM technology during exercise, lag time is long and accuracy is poor — it takes a while for the CGM to detect the current blood glucose value and it overestimates it. So, if the CGM says you are hypoglycemic then you probably have been for at least several minutes
To summarise the above… At present, no evidence supports the notion that knowing your glucose levels real-time during exercise will increase your performance. There is no evidence that having a higher blood glucose concentration makes you faster. There is also zero evidence that “glucose performance zones” exist or have any real-world utility. And, blood glucose is not a “fuel gauge” (except during hypoglycemia).
That is quite a damning opinion.
But, I am not all doom and gloom. There is something quite positive...
Alex Hutchinson also recently wrote about how British elite runner, Jake Smith, was told “you need to eat more”, based on his pre-race and during-race blood glucose levels. Furthermore, Smith’s glucose levels were so high during a half-marathon that they “maxed out the sensor throughout the race”. Remember that Supersapiens’ CGM only measures up to 200 mg/dL (~11 mmol/L). Also remember that CGM accuracy is poor during exercise and overestimates blood glucose.
What I find interesting is that these athletes are resorting to expensive devices to tell them that they need to consume food to maintain carbohydrate availability during exercise. My opinion is that if any sub-par race-day performances are due to inadequate nutrition and low carbohydrate availability, it does not require a CGM and data crunching to provide that information. Any good coach, physiologist, or nutritionist knows how to diagnose and remedy that issue without any fancy tech.
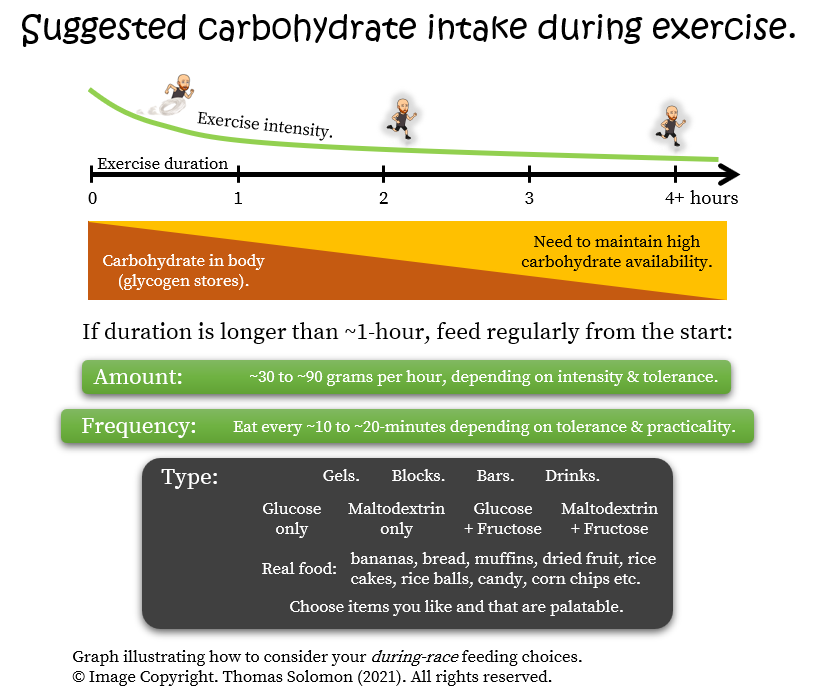
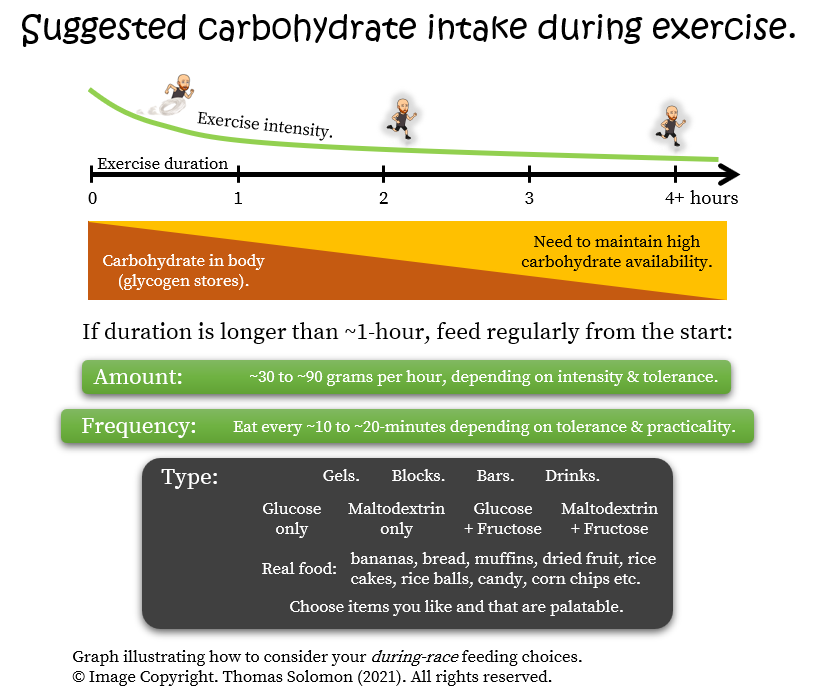
The evidence to date indicates that fueling long-duration high-intensity exercise “burns” stored carbohydrates (glycogen). The most efficient way to spare precious liver glycogen and “burn” for longer is to “fuel for the work required” by eating carbohydrates during a race or long arduous session — what a simple fix (see the animation below)
For some athletes and coaches who lack knowledge of nutrition, have trouble with during-race nutrition, and need some visual evidence of what happens to blood glucose when they try to train hard for many hours without food, a CGM might be a very useful tool. But, education on when, what, and how to eat during a race is already well-known, practiced during training, and implemented on race day by many athletes. The earliest knowledge on this topic emerged in ~1920 and nowadays we have highly detailed knowledge on how much fuel our bodies store, how long it allows us to go, how to establish high carbohydrate availability before exercise, and why you should consider maintaining carbohydrate availability during exercise...
To summarise 100-years of research and practice, you can educate yourself with a very simple framework that athletes have been using for at least 20-years:
 If your session or race is longer than ~1-hour,
If your session or race is longer than ~1-hour,
 Feed regularly from the start, every ~10 to ~20 mins, depending on tolerance and practicality.
Feed regularly from the start, every ~10 to ~20 mins, depending on tolerance and practicality.
 Consume ~30 to ~90 grams of carbs per hour, depending on intensity and tolerance.
Consume ~30 to ~90 grams of carbs per hour, depending on intensity and tolerance.
 Choose from a variety of sources, including fluids, gels, blocks, bars, or real food.
Choose from a variety of sources, including fluids, gels, blocks, bars, or real food.
 Pick items you like and find palatable when unleashing your war face.
Pick items you like and find palatable when unleashing your war face.
 Having more data doesn’t mean better. Sometimes, less is more.
When choosing any fancy gadget, always be mindful that obsessing over data metrics when you do not have the tools and/or knowledge to be able to appropriately interpret and respond, is like trying to punch the wind.
Having more data doesn’t mean better. Sometimes, less is more.
When choosing any fancy gadget, always be mindful that obsessing over data metrics when you do not have the tools and/or knowledge to be able to appropriately interpret and respond, is like trying to punch the wind.
To give a CGM to a nondiabetic athlete, telling them that they need to stay in a “glucose performance zone” and telling them that blood glucose = a fuel gauge is, to put it kindly, utter nonsense. Until thorough independent validation studies are conducted, and until during-exercise CGM accuracy improves, and until a body of evidence indicates that higher blood glucose = better performance, my opinion is that, CGM for athletes is all hype.
Accordingly, the three things I find important are:
 CGMs should be affordable or free to those who actually need them — people with diabetes.
CGMs should be affordable or free to those who actually need them — people with diabetes.
 The amount of plastic waste produced by disposable CGMs is bonkers. If CGM is essential then let’s minimise its use to those who need them — people with diabetes.
The amount of plastic waste produced by disposable CGMs is bonkers. If CGM is essential then let’s minimise its use to those who need them — people with diabetes.
But, most relevant to this conversation, is...
 Making athletes stress over their blood glucose levels and more arbitrary “zones” while educating them to keep blood glucose as high as possible at rest and throughout exercise is, at best, completely uninformed by evidence and, at worst, may create unhealthy eating practices and unnecessary pathology.
Making athletes stress over their blood glucose levels and more arbitrary “zones” while educating them to keep blood glucose as high as possible at rest and throughout exercise is, at best, completely uninformed by evidence and, at worst, may create unhealthy eating practices and unnecessary pathology.
As with any topic, I am certainly open to changing my mind but only if a body of evidence emerges. And, as I said, if seeing your blood glucose tumble during a race is the nudge you need to learn about carbohydrate availability, then great! But, until that day, I can suggest plenty of other things to “waste” €150 a month on… A reputable textbook (e.g. this or this) to educate yourself about sports nutrition, or a consultation with a sports nutritionist. Or, spend nothing at all, except “buying me a beer” after you’ve dug into my treasure trove of free sports nutrition deep dives at veohtu.com/articles. Be a nerd — educate yourself today, race better tomorrow!
Thanks for joining me to hear my opinion. I am passionate about equality in access to free education. If you find value in my content, please help keep it alive by sharing it on social media and buying me a beer at buymeacoffee.com/thomas.solomon. For more knowledge, join me @thomaspjsolomon on Twitter, follow @veohtu on Facebook and Instagram, subscribe to my free email updates at veothu.com/subscribe, and visit veohtu.com to check out my other Articles, Nerd Alerts, Free Training Tools, and my Train Smart Framework. To learn while you train, you can even listen to my articles by subscribing to the Veohtu podcast.
Until next time, keep thinking outside the box to keep training smart.
Between 2009 and 2018, I used CGM devices in several clinical studies including ~150 subjects (see my CGM publications here). I started with Medtronic’s CGMS System Gold moving on to Medtronic’s Guardian and iPro2 models, and eventually transitioning to Dexcom’s G5 and G6 models. I have also worn all those models in pilot testing for said studies. More recently and more relevantly, I have used Abbott’s Libre Sense Glucose Sport Biosensor (the CGM being used by Supersapiens). Furthermore, I spent my entire academic career studying human metabolism, nutrition, and exercise physiology, with a specific focus on glucose metabolism and blood glucose control — I have over 80 publications on this topic. I am also a coach. And, although I no longer consider myself an athlete, I continue to train and occasionally race. The bottom line... I am very familiar with CGM technology, have witnessed its development, understand its limitations, have a deep understanding of glucose metabolism and how it applies to training as a practitioner and a doer; and, most importantly, am not sponsored by, affiliated with, or receiving royalties from either Abbot, Dexcom, or Medtronic. Forever and ever, Amen.
Right with that out the way…
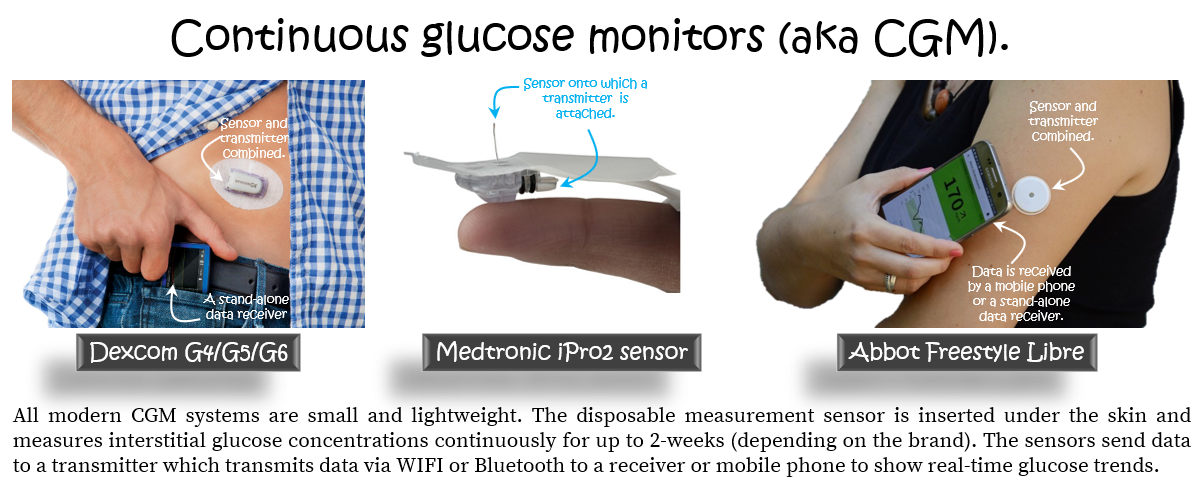
What is continuous glucose monitoring (CGM)?
A CGM device is a lump of plastic that sits on the skin with a tiny hair-like sensor inserted under the skin (i.e. subcutaneous) that continuously detects glucose concentrations in the interstitial fluid (not in your blood and not in your tissues but somewhere in the space between). Some devices (Dexcom) are about the size of a small lego brick, other devices (Abbot and Medtronic) are like a large coin. The sensors measure glucose approximately every 1- to 5-mins for up to 14-days (depending on the brand/model) and are then discarded. Some models (Abbot) have a built-in and disposable data transmitter, while other models (Dexcom and Medtronic) have multi-use transmitters into which you plug new sensors as needed. The transmitters wirelessly send glucose data to a receiver or a mobile phone.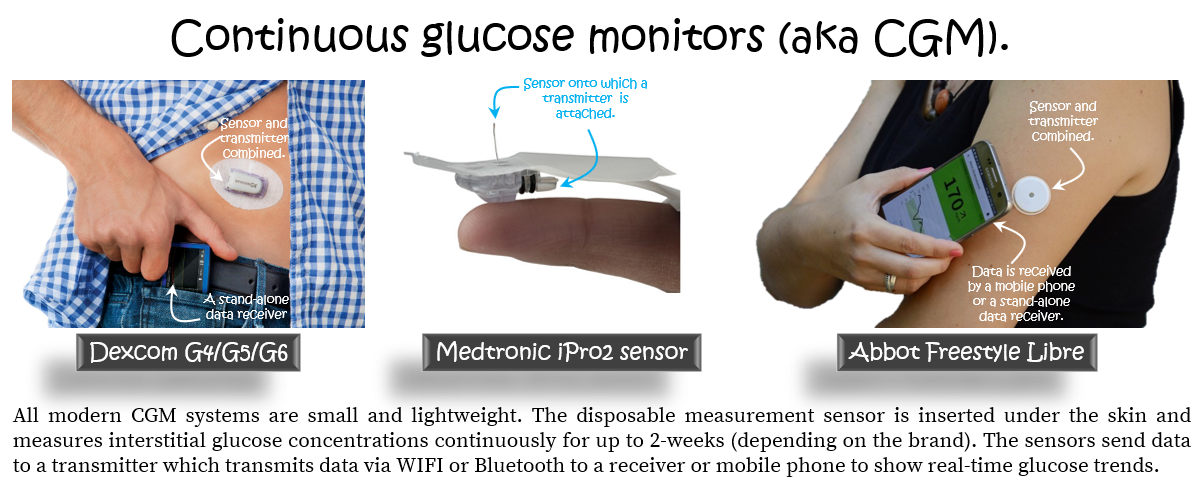
×
![]()
The glucose concentrations can be continuously visualised and provide an estimate of what is happening in your blood. This is important because changes in blood glucose concentrations reflect the balance between glucose leaving the blood and glucose entering it. At rest, if you are healthy, your blood glucose is around 5 mmol/L (or 90 mg/dL in USA units). If you eat a carbohydrate-containing meal, this value rises a little (to ~6-8 mmol/L or 110-180 mg/dL) and falls back towards baseline within an hour or so depending on the size of the meal. If you have diabetes, your resting blood glucose value is higher (above ~7 mmol/L or ~126 mg/dL) (because the liver throws more glucose into the blood than other tissues remove from the blood) and after a carbohydrate-containing meal, your blood glucose rises (above ~10 mmol/L or 200 mg/dL) and stays high for far longer than someone without diabetes (because less glucose is removed from the blood due to absent/insufficient insulin secretion [all types of diabetes] and due to poorer tissue sensitivity to insulin [type 2 and gestational diabetes]).
Persistently high blood glucose is undesirable because constantly exposing your organs to excessively high glucose triggers molecular events that massively increase the risk of a whole host of undesirables — stroke, heart attack, dementia, retinal failure, kidney failure, nerve failure, and so on…
Reducing persistently-elevated blood glucose levels in folks with diabetes drastically reduces their risk and improves their quality of life. People with diabetes — including athletes with diabetes — achieve this by managing their blood glucose with diet, exercise, and a menu of glucose-lowering drugs, including insulin.
Sweet.
CGM can help people with diabetes monitor blood glucose to help optimize their feeding, activity, and insulin dosages. Therefore, CGM can help folks learn to manage their diabetes while providing doctors with prognostic information. Sounds amazing. But, with any tool, it is always important to understand what the data tells you and what its limitations are. So...
What data do you get from a CGM?
Using an app or by open-source software (e.g. EasyGV, a research tool; or Nightscout and Tidepool, clinical tools made by patients for patients), data analysis is simple. But, you can extract a huge number of metrics that can be confusing and overwhelming. However, the information boils down to two key pieces of information:Glucose exposure.
— in the past 24-hours, how much glucose, on average, have your organs been exposed to? Typically assessed with the mean (or average) glucose, for which “too low” (aka hypoglycemia, less than ~4 mM or 70 mg/dL) is equally as bad as “too high” (aka hyperglycemia, greater than ~8 mM or 140 mg/dL); and the time in range, i.e. the time spent in the healthy range above the hypoglycemic threshold and below the hyperglycemic threshold.And
Glucose variability.
— in the past 24-hours, how much fluctuation was there? E.g. the standard deviation (or spread) of glucose concentrations around the mean (or average) glucose concentration.The limitations of CGM.
When I first used CGM in the late 2000s, the glucose sensors were connected via a wire to a data receiver, which you clipped onto your belt — it was clumsy. Plus, they hurt to insert and were irritating to wear. Nowadays, the sensors are very small, almost painless to insert, minimally uncomfortable, are Bluetooth or NFC connected to a smart device, and the data is easy to view and simple to analyse.Progress!
But, there are some limitations...
Firstly, due to the uncertain cost-effectiveness economics — i.e. simply having a CGM does not make a person’s diabetes disappear — healthcare systems do not dish CGMs out to all patients. Typically only folks who can afford it or those who can afford health insurance that covers it, get their mitts on a CGM. For example, the Medtronic iPro2 is ~€250 every 4-weeks (4 × 1-week sensors) plus ~€1200 upfront for the transmitter unit (which lasts forever) while the Dexcom G5/G6 is ~€250 for 4-weeks (4 × 1-week sensors) plus ~€250 every 3-months for the transmitter unit.
Secondly, to measure the concentration of glucose (or any metabolite) circulating in the blood (or, more accurately, the blood plasma, the “water” fraction of blood in which metabolites are dissolved, or even more accurately, the interstitial fluid between the blood and your tissues, in the case of CGM), we need three things:
And/or
Thirdly, while CGM accuracy (or MARD) is acceptable, its precision is questionable… Initially, evidence supported CGM in helping people establish “personalised nutrition” (see here, here, and here). But, when different meals are ranked according to their blood glucose response, the within-person variability of glucose responses to the same meals is huge. Furthermore, CGM devices from different companies rank meals in a very different order. This means that the error of measurement of CGM as a biomarker for blood glucose is rather large and is not just caused by consistent error (bias) but also variable error (aka noise). Such poor precision may lead to imprecise nutritional decisions.
And, lastly, if you have ever worn and/or seen data generated by a CGM, you will know that the data is not smooth eye-pleasing curves of glucose climbing and falling — biology is erratic. Meal-to-meal glucose responses are not consistent and you have to be careful to avoid “availability heuristics” that bias your interpretation and make you believe that “what you see is all there is”. For example, if you just ate white bread and glucose goes up, this does not mean that you should never eat white bread. Furthermore, if you ate white bread today and the response was smaller than it was yesterday does not mean that you are healthier today. Consequently, the major limitation of CGM is that to interpret CGM data and respond to it appropriately, you need knowledge of nutrient metabolism and behavioural psychology.
×
![]()
As you can see, CGM is far from perfect. CGM gets close to the true value (decent accuracy) but doesn’t always hit the same value (less-than-ideal precision). And, that is at rest and during meals. So, the next important question to ask:
Is CGM accurate and precise during exercise?
During exercise, things are very different — there are large and rapid changes in both the amount of glucose appearing in the blood (from the liver) and large plasma volume shifts (due to dehydration). So, we must question whether CGM can hit the true glucose value and/or the same glucose value every time it spits a number on the screen.Now is a good time to mention that, in the clinical world of diabetes, using CGM for assessing blood glucose during exercise is an area of debate...
The first thing to note is the time lag between changes in blood glucose (which is what your body is exposed to) and interstitial glucose (which is what CGM measures). The current evidence shows that CGM accuracy (or MARD) during higher intensity exercise is poorest during the earlier stages of a bout, even in the newest models. But, this does not imply that CGM is bad but it is important for people with diabetes because if CGM glucose is low during exercise it means their actual blood glucose is likely lower. Consequently, patients who suspect hypoglycemia during exercise are advised to confirm glucose with an accurate and precise finger prick measurement rather than relying on what the CGM is telling them.
Some studies show that CGM accuracy is reasonable during low-intensity walking (on average, MARD is ~17% when a 30-min walk starts after a meal and ~19% when walking before eating, using a FreeStyle Libre device). But during more vigorous exercise, MARD values for FreeStyle Libre start to inflate. For example, in one study, on average, MARD was ~30% during 45-minutes of moderate-intensity exercise.
To help put these values in context, a MARD value of 30% means that the CGM-measured value is 30% higher than the current blood glucose value, i.e. when blood glucose is truly 100 mg/dL (~5.6 mmol/L), the CGM gives a value of 130 mg/dL (or ~7.3 mmol/L). This can be a problem for people with diabetes because hypoglycemic blood glucose values below 70 mg/dL (~4 mmol/L) during exercise, would be indicated as “within the healthy range” on the CGM.
Other brands have been found to perform a little better. For example, the Dexcom G6 has shown slightly better and more consistent accuracy during fixed-intensity aerobic (MARD: 8.9 to 13.9%), interval (12.1 to 16.8%), and resistance (7.7 to 14.5%) exercise bouts. But, in 2021, Da Prato and colleagues evaluated several devices simultaneously, finding that CGM accuracy during exercise was generally poor for all devices, MARD ranging from 16% to 28% to 30% to 45%, depending on devices and types of exercise.
But perhaps I am cherry-picking studies?
Fear not… In 2021, Fabra et al. systematically reviewed the evidence for several Medtronic, Dexcom, and Abbot devices. Their meta-analysis showed massive variability between devices and that CGM devices overestimate blood glucose during exercise compared to rest with a moderate effect size of 0.35. They concluded that “the more recent sensor used, the better the technology and more accurate the CGM devices are”, which is encouraging.
×
![]()
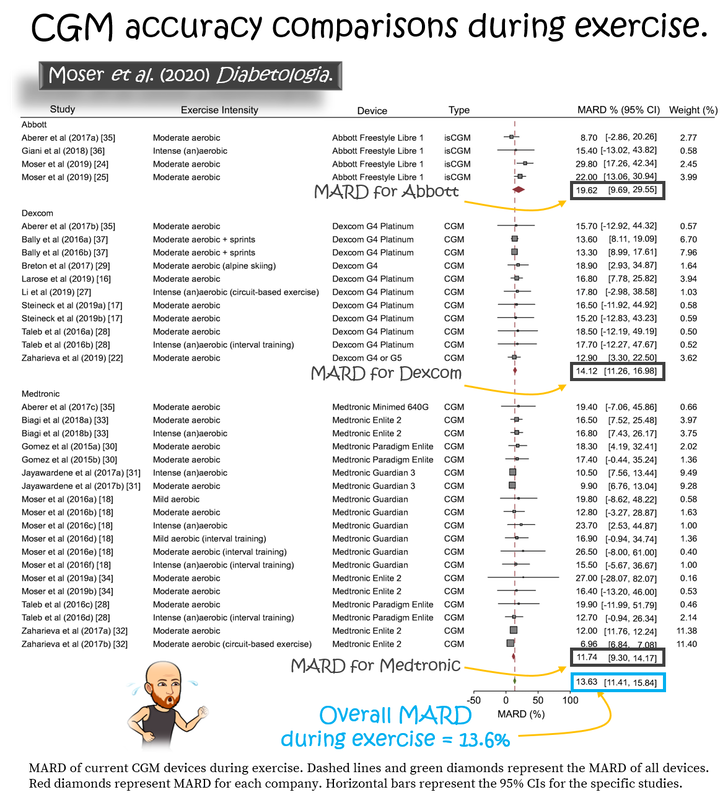
These concerns are echoed in a 2020 position statement from EASD (European Association for the Study of Diabetes), ISPAD (International Society for Pediatric and Adolescent Diabetes), JDRF (Juvenile Diabetes Research Foundation), and ADA (American Diabetes Association), which used a meta-analysis to show that MARD during exercise is poorer for Abbot devices (19.6%) than for Dexcom (14.1%) or Medtronic (11.7%).
×
![]()
While CGM accuracy (as measured using MARD) has been studied intensively, there is no data on precision during exercise. It is also important to note that the vast majority of studies have been conducted in patients with type 1 diabetes, i.e. in folks with large daily ranges in blood glucose, not in healthy athletes. The current evidence tells us that, during exercise, your CGM will miss the true blood glucose value by about 14%, on average. The evidence also indicates that Abbott’s current Freestyle Libre devices (upon which Supersapians is built) have poorer accuracy than devices from Dexcom and Medtronic. If this 14% “inaccuracy” is consistent for every measure, then we could say that this is acceptable. But, if your CGM does not always hit the same value — is imprecise — “acceptable” accuracy becomes less acceptable because without knowing how precise your CGM is during exercise, its accuracy is rather meaningless. In other words, an accurate but imprecise tool might not be a useful tool when wanting to make daily decisions about your carb intake during exercise. Since, you’ve already learned that CGM precision is rather poor at rest and during meals, this does not bode well for the potential precision of CGM during exercise. No doubt, research will shed light on this very soon.

×
![]()
Now I hope the concept of CGM is clear and that you understand its limitations. Given what we know about CGM accuracy during exercise, I also hope you can appreciate my initial scepticism about the utility of CGM for informing fueling decisions during exercise in nondiabetic athletes. But, let’s delve deeper...
CGM use in athletes. Welcome to Supersapiens and their “glucose performance zone”.
A new CGM device, Abbott’s Libre Sense Glucose Sport Biosensor, is being marketed at athletes by Supersapiens. It costs ~€150 for 4-weeks (2 × 2-week sensors) and is built on the same technology as Abbott’s Freestyle Libre CGM with some alterations — the glucose range is narrower (50 to 200 mg/dL, or ~3 to ~11 mmol/L) and, therefore, not suitable for people with diabetes, and its operating temperature only goes down to 10°C, so don’t plan on using it in the cold.They aim to revolutionise fuelling in sport using a “Glucose Performance Zone” concept, claiming that real-time blood glucose measurements act as a “fuel gauge” and claiming that high blood glucose equals lots of fuel in the tank, which equals you will go faster. Their marketing is slick and the idea sounds pretty punchy. Investors certainly thought so — initial capital searching raised $13.5 million! Plus, they are using the very clever “Maurten marketing model” of using big investment income to sponsor as many big names in endurance sport as they can to endorse their product. For example, Supersapiens is the new title sponsor of Ironman World Champs in Hawaii and have sponsorship-contracts with pro cycling teams, Ineos Grenadiers and Jumbo Visma, the great Eliud Kipchoge and hundreds (!) of other athletes.
It is very impressive. But, you’ve probably guessed that I am not mesmerized by their narrative (and nor were the UCI who, in 2021, banned the use of CGM during cycling races, partially upholding their “no needle” policy).
Why the negative mood, Solomon?
Well, to start, their “Glucose Performance Zone” and “fuel gauge” concepts are not supported by any evidence. This might sound surprising since Supersapiens has published several blog articles highlighting the “evidence” (for examples, see “The Close Ties Between Glucose Levels and Athletic Performance” and “Go Faster Longer: Use CGM To Know What Glucose Levels You Should Maintain To Maximise Your Training” and “Glucose Zones: Where To Manage Your Glucose Levels To Reduce Inflammation And Promote Recovery”). But, their home page and “education hub” blog pages don’t cite any actual evidence. Yes, these pages look impressive with lists of citations but the act of listing scientific papers is not a goldpass for supporting evidence.
When you scratch beneath the surface, Supersapiens have simply used an approach that many students have tried to slip under my radar in their assignments — they refer to papers that merely mention the topic in question rather than papers that test relevant hypotheses and generate relevant data. I will get to the actual evidence in a moment, but the “scientific theory” they have compiled is shoddy and the narratives are written simply to fit the goal of the product. That is, after all, how many companies sell us new products. But, if they were a student in my class, they’d get a D-grade and some notes on how to use published evidence.
Beyond that, I also fear Supersapiens are promoting unhealthy eating practices. One of their recent blog posts (“Fresh Take On Fuelling”) says: “A bowl of gels for breakfast is not conventionally accepted as a good start to the day, yet we seem to find this ideal when exercising in the morning.”. As an academic, coach, former athlete, and human who cares about people’s performance AND health, this truly gets me tugging at my ginger beard. No athlete should swap healthy whole foods for gels at any meal, ever. I suspect there is probably a Supersapiens-Maurten collaboration on the horizon… Anyway, enough about that...
Does high blood glucose mean lots of fuel in the tank and faster speeds?
Well, the best way to start answering that is to consider:What happens to blood glucose during exercise?
During exercise, your muscles start gobbling large amounts of glucose from the blood to maintain energy production. If your body did nothing about this, hypoglycemia would occur in minutes. But your liver is awesome and responds preemptively to keep you rocking...
One fundamental aspect of human physiology Supersapiens have overlooked is the effect of “stress” on liver glucose output. In this context, exercise — a physical stress — increases adrenaline release, causing a glucagon response that increases glucose output from your liver. This is part of your fight or flight response that helped your ancestors successfully deliver you to your place on Earth. In fact, one of the key life-saving tools for a type 1 diabetic athlete who is plunging into hypoglycemia during exercise when they don’t have food available is to do some sprints. Why? Because the high intensity triggers adrenaline release and a subsequent rapid release of glucose from the liver into the blood. But this doesn’t only occur in diabetic patients. This fundamental biology occurs in all of us.
What is my point?
Well, if you go do anything with intermittent bursts of high intensity and you are wearing a CGM, you will see that your blood glucose will rise as you start your warm-up and probably spike intermittently as you unleash your mayhem. This is fundamental biology that was discovered long before I was delivered to Earth 41 years ago.
During interval sessions and weights sessions AND during prolonged hard races, your “fuel tank” (aka glycogen) is continuously depleted. Stored glycogen in your muscles and your liver slowly decrease but blood glucose does not. In fact, during a prolonged high-intensity race you will see your blood glucose rise and remain above baseline concentrations.

×
![]()
During exercise, the only time when you’ll see your blood glucose continually drop is when your liver glycogen is depleted. This can happen, for example, when you start exercise with low glycogen levels (fasted exercise), or when you exercise at an intensity that requires a high carbohydrate availability (a marathon), or when you exercise for a long time (an ultra). Even when muscle glycogen is depleted, blood glucose will be good until liver glycogen also dries up.
Blood glucose is not a biomarker for glycogen except perhaps when glycogen levels are depleted and blood glucose is the only food your muscles have to keep on rocking. For this reason, blood glucose during exercise tells you nothing about your “fuel tank” nor, therefore, can it be a “fuel gauge”. So, what will continuous blood glucose readings during exercise tell you about performance?
Not much.
But, that is just my narrative. An important question is...
What is the evidence for using CGM for fueling exercise performance?
When scientists at Harvard studied athletes in the Boston marathon in the 1920s, we began to understand that carbohydrate intake during prolonged races can be a useful performance tool (I reviewed that work here). A century later, it is very clear that during-race carbohydrate feeding helps resist fatigue during races. (For a thorough review of all the evidence, please see my 6-part deep-dive on performance nutrition and my summary figure here.)But how do CGMs fit into this story?
Back in May, I ran a self-supported 60 km loop in my local mountains with ~2000 metres of elevation gain and loss. I ate 353 kcals per hour, including 76 grams of carbs per hour, and with Abbott’s Libre Sense Glucose Sport Biosensor — Supersapiens — I collected CGM data throughout but blinded myself to the data and, therefore, it did not inform my feeding choices. My average glucose was 134 mg/dL with a glucose variability (standard deviation) of 9 mg/dL and a range of 110 to 161 mg/dL. Since it's not possible to download the raw Supersapiens data, I could only visually compare my blood glucose concentrations with my grade-adjusted pace during the run — there was no apparent relationship.
But that is just a bias-filled anecdote from personal use. What about objective studies?
In 2015, Sengoku and colleagues used Medtronic’s System Gold CGM to observe blood glucose in 2 ultrarunners during a 100 km race. During the race, blood glucose gradually increased but, while the faster of the two racers maintained their blood glucose throughout the race, the slower runner had a sharp drop in their blood glucose eventually resulting in hypoglycemia (less than 70 mg/dL or ~4 mmol/L), despite similar during-race feeding habits.
In 2020, Kengo Ishihara and colleagues published a similar observational study using Abbott’s FreeStyle Libre CGM to monitor blood glucose in 4 male and 3 female ultrarunners during a 160 km mountain race. By the end of the race, runners’ average glucose concentration rose from ~104 to ~164 mg/dL (~5.8 to ~9.1 mmol/L) and the total amount of carbohydrate intake during the race ranged from 16.3 to 52.9 g/h. Runners did not use the CGM to inform their feeding decisions but a greater carbohydrate intake positively correlated with faster running speeds (R2=0.80 and P=0.007, which means that 80% of the variance in speed was explained by the amount of carb intake and that there is a measly 0.7% chance that this strong association is due to random chance) and those with higher carb intake better maintained their blood glucose during the race.
But, was blood glucose correlated with race speed?
Yes, but with nuances...
Rather than simply comparing the average (mean) blood glucose and the spread (standard deviation) of values with running speed, they compared the change in glucose (end of race minus baseline) vs. speed and then stratified the changes into arbitrary “lowest”, “average”, and “largest” changes (without defining what lowest, average, and largest mean). This is an odd “data mining” analysis, especially when you only have 7 subjects, because it screams, “we were fishing to find significance”. Anyway, they found that the “lowest” (males: R2=0.24, P=0.003; females: R2=0.14, P=0.05) and “average” (males: R2=0.17, P = 0.02; females: R2=0.05, P = 0.24) glucose changes were positively related to faster speeds but that the “largest” change in glucose was not (males: R2=0.0005, P=0.90; females: R2=0.01, P=0.57). Yikes, that is confusing.
In 2021, another observational study of 1 female athlete racing a 438 km FKT around Lake Biwa was published in 2021 by the same group. Using Abbot’s Freestyle Libre, they found that her average daytime and nighttime blood glucose were ~130 and ~125 mg/dL. By dividing the distance into 32 segments, the authors found that her running speed was associated with total energy (P=0.02) and carbohydrate intake (P=0.01), specifically for solid foods vs. liquids and gels, but that her blood glucose concentrations did not correlate with running speeds.
×
![]()
While there are a couple of other studies (see here) that have used CGM to examine glucose control following meals in athletes, the studies I have discussed are all that currently exists where CGM is used to examine the association between blood glucose during exercise and exercise performance.
Why do Supersapiens not cite them?
Perhaps because the studies do not support their “glucose performance zone” or “fuel gauge” narratives. Instead, these studies simply use real-world and meaningful race day conditions to confirm what we already knew:
Is blood glucose a “fuel gauge”?
Kind of. But, not really. And, definitely not in the sense that higher = faster. Let me explain..I previously went deep on this topic at veohtu.com/thefuelinyourbody, veohtu.com/burningfuelduringexercise, and veohtu.com/howlongcanyougo. But, to summarise that info, the fuel available to you during exercise can be conceptualised as:
My point is that your blood is simply a “vessel” in which glucose is transported between tissues. Despite the importance of glucose as the major fuel for hard work,
That said, when your blood glucose approaches hypoglycemic levels and drops below ~70 mg/dL (~4 mmol/L), a different story emerges. Hypoglycemia can hint that accessible fuel is low — during exercise, hypoglycemia typically indicates that your liver glycogen is low and/or you have exceeded your liver’s capacity to produce “new” glucose. And, now you're in trouble because if blood glucose keeps falling, fatigue signals will be sent to your brain and you will very likely succumb to Darth Fader (the Sith Lord of fatigue) and slow down.
When Supersapiens write enticing statements like “Average Glucose is naturally regulated around 90-110 mg/dL, but may need to be higher for you leading into a training or performance event”, they are just using the power of suggestion. There is no evidence that you need to raise your fasting glucose level above baseline to increase performance. If we have learned anything about fueling during exercise over the last 100-years it is that we do not and should not wait for blood glucose to change to consider a fueling choice. When blood glucose drops too low, you will be in trouble. Plus, what we currently know about CGM technology during exercise, lag time is long and accuracy is poor — it takes a while for the CGM to detect the current blood glucose value and it overestimates it. So, if the CGM says you are hypoglycemic then you probably have been for at least several minutes
To summarise the above… At present, no evidence supports the notion that knowing your glucose levels real-time during exercise will increase your performance. There is no evidence that having a higher blood glucose concentration makes you faster. There is also zero evidence that “glucose performance zones” exist or have any real-world utility. And, blood glucose is not a “fuel gauge” (except during hypoglycemia).
That is quite a damning opinion.
But, I am not all doom and gloom. There is something quite positive...
CGMs are revealing that some athletes and coaches have poor knowledge of sports nutrition.
Professional athlete’s comments on the Supersapiens website include things like:
“A huge positive change I tested and now stick to daily is making sure I eat between 75-120 grams of carbs per hour on the bike. Riding where it’s hot and humid, the body is working really hard to not only maintain itself, but to be used for intense intervals or long hours. Fuelling adequately and often is my number one take away from looking at the insights I received from the Supersapiens app.”
Alex Hutchinson also recently wrote about how British elite runner, Jake Smith, was told “you need to eat more”, based on his pre-race and during-race blood glucose levels. Furthermore, Smith’s glucose levels were so high during a half-marathon that they “maxed out the sensor throughout the race”. Remember that Supersapiens’ CGM only measures up to 200 mg/dL (~11 mmol/L). Also remember that CGM accuracy is poor during exercise and overestimates blood glucose.
What I find interesting is that these athletes are resorting to expensive devices to tell them that they need to consume food to maintain carbohydrate availability during exercise. My opinion is that if any sub-par race-day performances are due to inadequate nutrition and low carbohydrate availability, it does not require a CGM and data crunching to provide that information. Any good coach, physiologist, or nutritionist knows how to diagnose and remedy that issue without any fancy tech.
The evidence to date indicates that fueling long-duration high-intensity exercise “burns” stored carbohydrates (glycogen). The most efficient way to spare precious liver glycogen and “burn” for longer is to “fuel for the work required” by eating carbohydrates during a race or long arduous session — what a simple fix (see the animation below)
To summarise 100-years of research and practice, you can educate yourself with a very simple framework that athletes have been using for at least 20-years:
×
![]()
What can you add to your training toolbox?
First off, I want to emphasise that I have been ranting about the use of CGM in athletes without diabetes. I am not disregarding the utility of CGM for people with diabetes, including athletes with diabetes, in whom CGM can be useful for detecting asymptomatic hypoglycemia during races. More specifically, I’ve ranted on the inaccuracy of CGMs during exercise and on the (non)existence and (lack of) utility of “Glucose Performance Zones”. To bring my rantiness back to some tangible take-home, consider this...To give a CGM to a nondiabetic athlete, telling them that they need to stay in a “glucose performance zone” and telling them that blood glucose = a fuel gauge is, to put it kindly, utter nonsense. Until thorough independent validation studies are conducted, and until during-exercise CGM accuracy improves, and until a body of evidence indicates that higher blood glucose = better performance, my opinion is that, CGM for athletes is all hype.
Accordingly, the three things I find important are:
But, most relevant to this conversation, is...
Thanks for joining me to hear my opinion. I am passionate about equality in access to free education. If you find value in my content, please help keep it alive by sharing it on social media and buying me a beer at buymeacoffee.com/thomas.solomon. For more knowledge, join me @thomaspjsolomon on Twitter, follow @veohtu on Facebook and Instagram, subscribe to my free email updates at veothu.com/subscribe, and visit veohtu.com to check out my other Articles, Nerd Alerts, Free Training Tools, and my Train Smart Framework. To learn while you train, you can even listen to my articles by subscribing to the Veohtu podcast.
Until next time, keep thinking outside the box to keep training smart.
Disclaimer: I occasionally mention brands and products but it is important to know that I am not affiliated with, sponsored by, an ambassador for, or receiving advertisement royalties from any brands. I have conducted biomedical research for which I have received research money from publicly-funded national research councils and medical charities, and also from private companies, including Novo Nordisk Foundation, AstraZeneca, Amylin, A.P. Møller Foundation, and Augustinus Foundation. I’ve also consulted for Boost Treadmills and Gu Energy on their research and innovation grant applications and I’ve provided research and science writing services for Driftline and Examine — some of my articles contain links to information provided by Examine but I do not receive any royalties or bonuses from those links. These companies had no control over the research design, data analysis, or publication outcomes of my work. Any recommendations I make are, and always will be, based on my own views and opinions shaped by the evidence available. My recommendations have never and will never be influenced by affiliations, sponsorships, advertisement royalties, etc. The information I provide is not medical advice. Before making any changes to your habits of daily living based on any information I provide, always ensure it is safe for you to do so and consult your doctor if you are unsure.
If you find value in this free content, please help keep it alive and buy me a beer:
 Buy me a beer.
Buy me a beer.
Share this post on your social media:
Want free exercise science education delivered to your inbox? Join the 100s of other athletes, coaches, students, scientists, & clinicians and sign up here:

About the author:
I am Thomas Solomon and I'm passionate about relaying accurate and clear scientific information to the masses to help folks meet their fitness and performance goals. I hold a BSc in Biochemistry and a PhD in Exercise Science and am an ACSM-certified Exercise Physiologist and Personal Trainer, a VDOT-certified Distance running coach, and a Registered Nutritionist. Since 2002, I have conducted biomedical research in exercise and nutrition and have taught and led university courses in exercise physiology, nutrition, biochemistry, and molecular medicine. My work is published in over 80 peer-reviewed medical journal publications and I have delivered more than 50 conference presentations & invited talks at universities and medical societies. I have coached and provided training plans for truck-loads of athletes, have competed at a high level in running, cycling, and obstacle course racing, and continue to run, ride, ski, hike, lift, and climb as much as my ageing body will allow. To stay on top of scientific developments, I consult for scientists, participate in journal clubs, peer-review papers for medical journals, and I invest every Friday in reading what new delights have spawned onto PubMed. In my spare time, I hunt for phenomenal mountain views to capture through the lens, boulder problems to solve, and for new craft beers to drink with the goal of sending my gustatory system into a hullabaloo.
Copyright © Thomas Solomon. All rights reserved.
I am Thomas Solomon and I'm passionate about relaying accurate and clear scientific information to the masses to help folks meet their fitness and performance goals. I hold a BSc in Biochemistry and a PhD in Exercise Science and am an ACSM-certified Exercise Physiologist and Personal Trainer, a VDOT-certified Distance running coach, and a Registered Nutritionist. Since 2002, I have conducted biomedical research in exercise and nutrition and have taught and led university courses in exercise physiology, nutrition, biochemistry, and molecular medicine. My work is published in over 80 peer-reviewed medical journal publications and I have delivered more than 50 conference presentations & invited talks at universities and medical societies. I have coached and provided training plans for truck-loads of athletes, have competed at a high level in running, cycling, and obstacle course racing, and continue to run, ride, ski, hike, lift, and climb as much as my ageing body will allow. To stay on top of scientific developments, I consult for scientists, participate in journal clubs, peer-review papers for medical journals, and I invest every Friday in reading what new delights have spawned onto PubMed. In my spare time, I hunt for phenomenal mountain views to capture through the lens, boulder problems to solve, and for new craft beers to drink with the goal of sending my gustatory system into a hullabaloo.
Copyright © Thomas Solomon. All rights reserved.