Education for runners and endurance athletes. Learn to train smart, run fast, and be strong.
These articles are free.
Please help keep them alive by buying me a beer:
 Buy me a beer.
Buy me a beer.
This article is part of a series:
→ Part 1 — How much fuel is in your body?
→ Part 2 — How do your muscles burn fuel?
→ Part 3 — How long can you go?
→ Part 4 — Carboloading
→ Part 5 — Race day carb availability
→ Part 6 — Putting it into practice
→ Part 1 — How much fuel is in your body?
→ Part 2 — How do your muscles burn fuel?
→ Part 3 — How long can you go?
→ Part 4 — Carboloading
→ Part 5 — Race day carb availability
→ Part 6 — Putting it into practice
Performance nutrition: Part 3 of 6:
How long does your body’s fuel stores allow you to go during exercise?
Thomas Solomon PhD.
22nd May 2021.
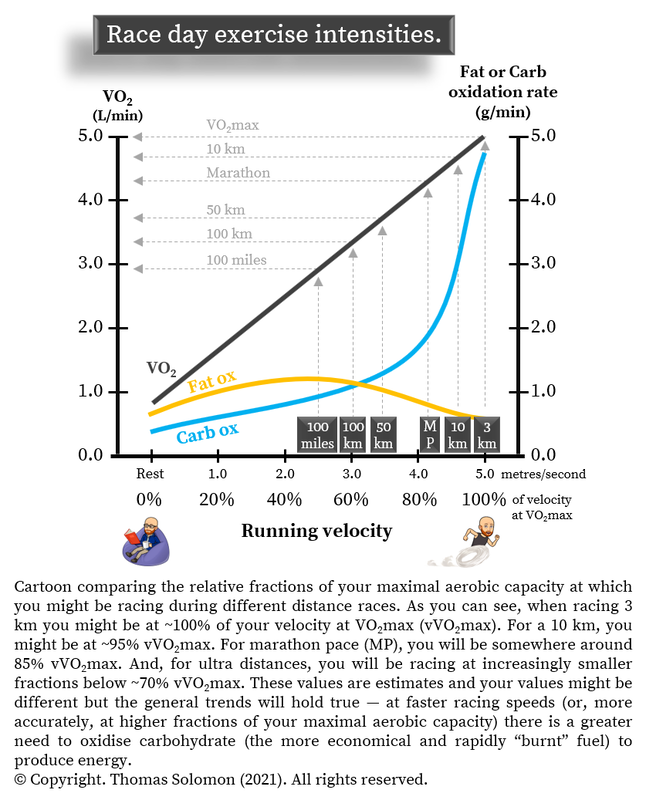
In part 1 of this series, you learned that your body’s two key fuel sources for endurance exercise are stored in different amounts — remember your bucket load of fatty acids and pint-glass of glucose. In part 2, you learned that with increasing exercise intensity — at increasing fractions of your maximal aerobic capacity (your VO2max) — your muscles develop a greater reliance on “burning” glucose and a lesser reliance on “burning” fatty acids to produce energy at the rate it is needed. Given what you have learned so far, it is time to consider how long your fuel stores will theoretically allow you to go at various running intensities.
Reading time ~20-mins (4000-words).
Or listen to the Podcast version.
Or listen to the Podcast version.
In this series on performance nutrition, I am focussing on bioenergetics and am not taking into account how, during exercise, your increasing body temperature, decreasing hydration status, decreasing muscle/connective tissue resilience, or decreasing motivation can each influence your feelings of fatigue and ability to maintain power output. These important determinants of your ability to keep on rockin’ are for a future discussion because, before tackling those complexities, it is important to consider how long your stored fuel allows your body to go.
Why?
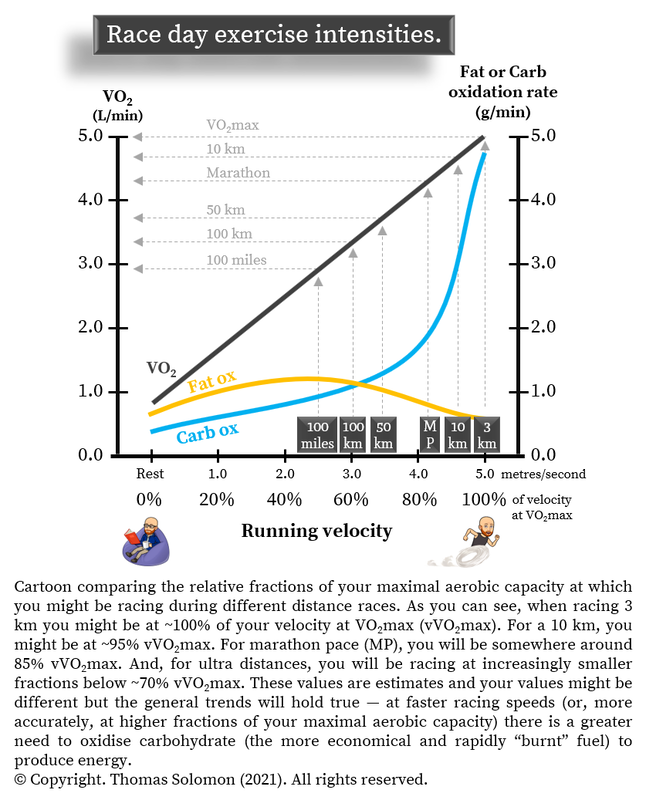
Because even at low to moderate intensities, like during an easy-effort run, when your muscles derive most of their energy from “burning” fatty acids, some energy still comes from “burning” a bit of glucose. Understanding this will help you conceptualise that both longer-duration races (raced at a lower fraction of your maximum aerobic capacity; VO2max) and high-intensity races (raced at a higher fraction of your VO2max, and therefore a higher speed) will eventually deplete your pint-glass of glucose despite having plenty left in your bucket load of fatty acids. Consequently, this framework will help you understand the need for performance nutrition to help you last the distance.
So, where do we start?
Well, since it is your muscles that are burning lots of fuel during exercise, let’s start with that part of the integrative physiology puzzle.
These were seminal observations but they did not provide clues as to why blood glucose fell.
In 1961, Reichard and colleagues used an intravenous infusion of radioactive 14C-labelled glucose to show that blood glucose is taken up into exercising muscle and “burned” to produce energy. The work also demonstrated that the loss of glucose from the blood into muscle is compensated by an increase in glucose release from the liver. In 1967, Jonas Bergström and Eric Hultman used muscle biopsies to show that prolonged exercise decreases muscle glycogen levels. By using arterio-venous catheterisation across the liver, they also found that the liver releases glucose into the blood during exercise but that its attempt to keep providing glucose to working muscles by releasing more glucose into blood during exercise is insufficient to match the total amount of glucose “burned” during exercise. Remember, your body always makes fuel available to the working muscle.
In the 1970s, the muscle biopsy technique became widespread. In the context of running, in 1971 Dave Costill’s work showed the progressive decline in muscle glycogen over 3-days caused by daily high-intensity running (10-miles/day). And, in 1973, he further demonstrated that a 30 km race, run at ~83% VO2max, caused a 30% reduction in the muscles’ fat store (IMTG) and a 60% reduction in muscle glycogen levels.
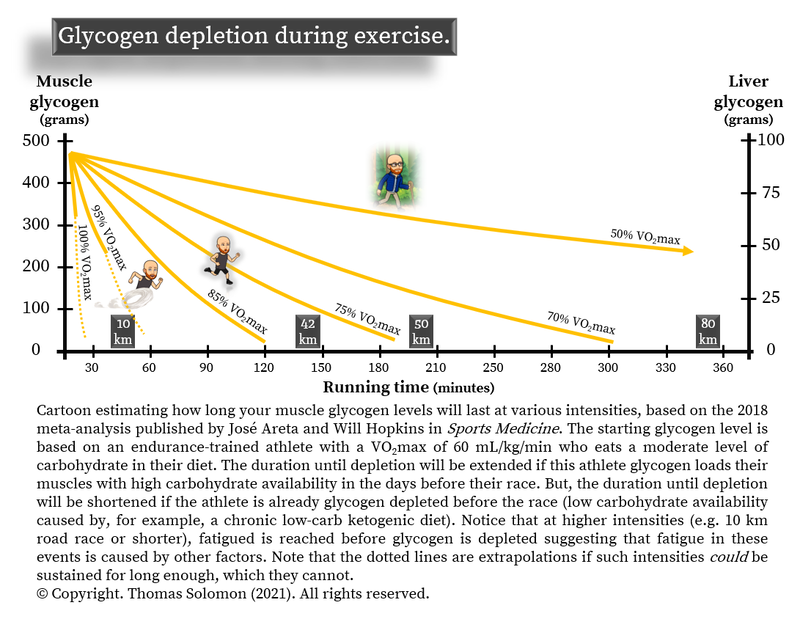
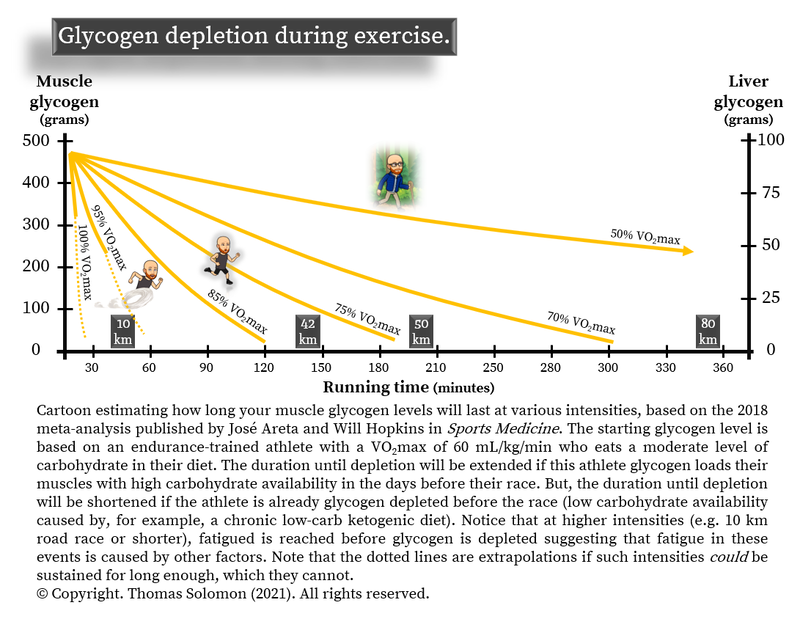
Many studies have since studied muscle glycogen utilisation during exercise and, nowadays, we are confident that prolonged exercise eventually depletes muscle glycogen. To help minimise any doubt in this sentiment, in 2018, José Areta and Will Hopkins published a beautiful meta-analysis of all known clinical data, showing that higher exercise intensity and longer duration exercise are the biggest predictors of the rate of muscle glycogen use. Furthermore, it is now clear that a low-glycogen state has a dramatic effect on whole-body metabolism — for example, glycogen depletion reduces the capacity to “burn” glucose, which will reduce our capacity to go fast, and increases muscle protein breakdown, which may affect recovery (reviewed in detail by Andy Philp and colleagues in 2012). Plus, more recently, we have come to appreciate that the depletion of specific glycogen “compartments” that are bound to contractile proteins cause reduced force production (reviewed by Niels Ørtenblad’s lab in 2013), directly implicating low glycogen with muscle fatigue. When someone reaches exhaustion through “glycogen depletion”, total muscle glycogen levels are never zero. Instead, we now know that depletion of specific depots of “available” glycogen occurs in type 1 (“slow-twitch”) muscle fibres during long-duration endurance exercise and in type 2 (“fast-twitch”) fibres during high intensity or strength exercise (see reviews here and here).
OK. It is probably now pretty clear to you that prolonged exercise depletes muscle glycogen. The next important questions is:
Many moons ago, Lars Nilsson & Eric Hultman used arterio-venous catheterisation across the liver to show that, in healthy folks, the liver throws glucose into the blood at about 0.15 grams per minute to help maintain normal blood glucose levels throughout the night, providing a constant fuel source for all your organs to feed on. They showed that about ½ of the liver glucose output during the first 10-hours of an overnight fast comes from liver glycogen breakdown while the other half comes from gluconeogenesis (aka “new glucose synthesis” from metabolites like glycerol, lactate, and amino acids). Such findings have been confirmed using less-invasive nuclear magnetic resonance spectroscopy methods, but these are energy costly processes that the liver cells fuel by producing energy from circulating fatty acids in the blood.
The liver can hold about 300 mmol/L of glycogen, which based on a liver volume of about 1.8 litres is equal to around 100 grams of glycogen. This amount varies little between trained athletes and untrained folks but it is related to the amount of carbohydrate eaten in the diet. It has also been known since the 60s that, in us human folks, an overnight fast massively depletes liver glycogen stores. To put that in perspective, since your liver releases glucose at ~0.15 grams per minute and about half of that comes from liver glycogen, then after a 10-hour overnight fast your liver glycogen level will be reduced to around 50-grams. But, in the 1970s, Nilsson & Hultman found that liver glycogen is rapidly restored with carbohydrate refeeding — one of the main reasons that humans eat a morning breakfast.
During exercise, the rate at which your muscles remove glucose from the blood goes waaay up — from ~0.13 to 0.16 grams per minute at rest up to ~1 to 1.5 g/min during exercise — a 6 to 10-fold increase in the amount of glucose leaving the blood every minute. And, every drop of glucose that enters muscle during exercise is “burned” — it doesn’t form new muscle glycogen. If you remember that the blood only contains about 4 grams of glucose, this means that if you did not have a liver, it would take only a few minutes for you to stop being “sweet” and the guillotine would drop. To prevent blood glucose levels from dropping — to prevent hypoglycemia — when your tissues are feasting on the blood’s sugary goodness, the rate of glucose release from the liver into the blood must also increase to maintain blood glucose levels within a healthy range (~1 g/L, or 5 mM). In 1967, Jonas Bergström and Eric Hultman used arterio-venous catheterisation across the liver to show that the rate at which the liver releases glucose into the blood increases in proportion to exercise intensity during exercise, from ~0.1 to ~0.4 g/min in an untrained person. Since then, several studies have examined this phenomenon using arterio-venous balance methods, stable isotopes, and 13C-NMR, and it is clear that large amounts of liver-derived glucose are “burned” by muscles during exercise (see here here, here, and here). Furthermore, during long-duration (~3-hours) moderate-intensity exercise (70% VO2max), liver glucose output into the blood can reach ~1 g/min in endurance-trained athletes.
However, this increase in liver glucose output comes at a cost:
Liver glycogen.
It is tricky to study liver glycogen in humans because of the high risk of using liver biopsies during exercise. So, alternative indirect methods with stable isotope tracers or arterio-venous balance measurements of glucose-producing substrates being taken up into the liver have been used to estimate glycogen synthesis rates. Fortunately, some studies have used modern 13C-NMR methods to measure changes in liver glycogen during exercise in endurance-trained athletes. In 2000, Anna Casey et al. showed that an 80-minute ride at 70% VO2max decreased liver glycogen by about 50% from ~120 grams to ~60 grams, and in 2016, Javier Gonzalez et al. found that following 3-hours of low-intensity cycling at 50% VO2max, liver glycogen decreased by about 40% from ~140 grams to ~90 grams.
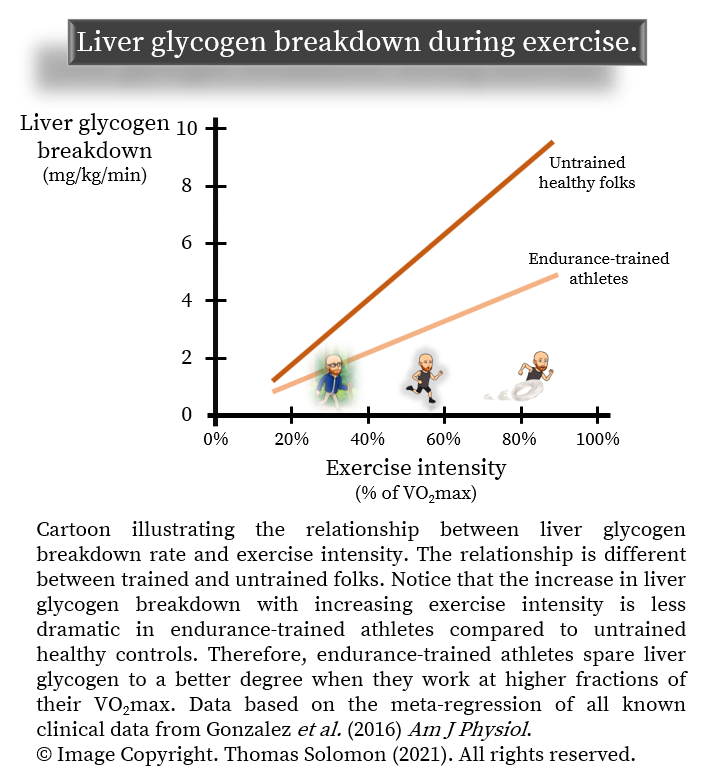
A meta-regression of all known clinical data by Javier Gonzalez clearly shows that the rate of liver glycogen depletion increases dramatically with increasing exercise intensity, but only in untrained folks. In endurance athletes, the rate of liver glycogen breakdown during exercise is lower than that of regular folks and rises to a lesser degree across a range of exercise intensities (see full table of studies here).
Yes, indeed. But there are a couple of caveats...
During exercise, the liver releases glucose into the blood and, in humans, this is predominantly from the breakdown of liver glycogen stores (rather than from gluconeogenesis of “new” glucose). Therefore, when liver glucose output is supporting moderate to high intensity exercise at a rate of 1 g/min, most of this glucose is coming from liver glycogen breakdown and, since your liver stores about 100 grams of glycogen, it will take about 100-minutes (1h40m) to completely deplete your liver glycogen store. Furthermore, let’s not forget that, during exercise, your liver tries its best to keep glucose — your economical and high-energy yielding fuel — available to the muscle. During the early stages of exercise, it is typical to see the liver release glucose into blood at a slightly higher rate than glucose is removed from blood (into muscle). Therefore, blood glucose levels often rise a little bit — there is a slight mismatch between glucose leaving and glucose entering the blood. But another mismatch occurs during prolonged exercise when liver glycogen levels become depleted. Then, the liver cannot release glucose at the rate needed to match the high rate of glucose uptake into muscle, which can be ~1 to 1.5 g/min during exercise.
The consequence?
If your liver glycogen “runs” out (pun entirely intended) and/or if your liver’s capacity to produce new glucose (via gluconeogenesis) is exceeded, blood glucose levels will begin to drop, resulting in hypoglycaemia, the signs of which are not pleasant — excess sweating, shivering, nausea, dizziness, etc. To put this in context, hypoglycaemia can arise if your race is long enough or intense enough or if your liver and muscle glycogen levels were already low to begin. When this happens, it is possible that hypoglycaemia likely acts as a “fatigue signal” to the brain — your rating of perceived exertion (RPE) goes up (exercise feels harder), your power output drops (you slow down), and you are soon forced to stop… probably because your clever brain wants to protect the beautiful body it needs so it can maintain a purpose in life. So, if your liver gets “tired” of producing glucose during exercise, your race plans will pretty quickly get eff dup. Your liver is awesome but it can only work so hard.
Note: For an excellent overview of how precious the few grams of glucose in your blood is, please read George Brooks’ 2020 narrative review. Or, for a visual representation of how this works, watch my animation below:
Hearing about glycogen depletion and hypoglycemia is all very depressing, so let’s turn our attention to something way more positive!
You also know that as you work harder, you use relatively more glucose than fatty acids to fuel your forward progress. Because of the limited size of your bodily carbohydrate store, it is very wise to assume that you are “metabolically” limited in how long you can proceed before fatigue sets in. And, as I mentioned at the beginning of this post, this is without even considering other important contributors to fatigue like training status, hydration, body temperature, or motivation, etc.
During an Easy-effort low-to-moderate-intensity run (i.e. 60% VO2max), your body is merely “drip feeding” from its carbohydrate stores (glycogen) at a rate of ~1 gram per minute, and so it will take a few hours to deplete your glycogen stores to critical levels. On the contrary, during very high intensities (i.e. above 90% and even beyond 100% VO2max), which might include races from 800m up to 10 km, your glycogen stores are gobbled at much higher rates. But, at such high intensities, you will not deplete them to critical levels because other factors (like metabolic acidosis) will limit the duration you can work for before you reach fatigue. Where the double double toil and trouble starts to bubble is during longer duration events, where you can operate at high intensities (e.g. 70 to 90% VO2max) for durations that will deplete your glycogen stores within a couple of hours. Most folks can “squeeze” in a road half-marathon (~1 to 2-hours) before they get a visit from Macbeth’s witches but when racing for longer than around 90-minutes — 16-milers, marathons, trail races, obstacle races — glycogen depletion is a high-risk affair.
Using what you have learned so far, I will now throw you into some basic maths to help contextualize how long you can theoretically keep on rocking, from a metabolic point of view.
Let’s imagine that Bob is a well-trained club-level athlete who generally eats a moderately high carbohydrate diet, and on marathon race day — where he aims to “compete” not merely “complete” — he has eaten a carbohydrate-containing breakfast.
At his marathon pace,
 Bob’s estimated whole-body fat oxidation rate is 0.5 grams per minute
Bob’s estimated whole-body fat oxidation rate is 0.5 grams per minute
and his
 whole-body carbohydrate oxidation rate is 4 g/min.
whole-body carbohydrate oxidation rate is 4 g/min.
At marathon pace, ~80% VO2max, muscle glycogen will account for about 75% of whole-body carbohydrate “burning”. So, Bob’s.
 muscle glycogen breakdown rate is 3 g/min.
muscle glycogen breakdown rate is 3 g/min.
The remaining 25% of whole-body carbohydrate “burning” will be supported by blood glucose uptake and oxidation. Therefore, his
 muscle glucose uptake rate (from blood) is 1 g/min.
muscle glucose uptake rate (from blood) is 1 g/min.
To maintain blood glucose levels, the liver will have to match this. So, Bob’s
 liver glucose output rate (into blood) is also 1 g/min (perhaps higher).
liver glucose output rate (into blood) is also 1 g/min (perhaps higher).
And, since most liver glucose output during exercise comes from glycogen, Bob’s
 liver glycogen breakdown rate is close to 1 g/min.
liver glycogen breakdown rate is close to 1 g/min.
So, what does all this mean?
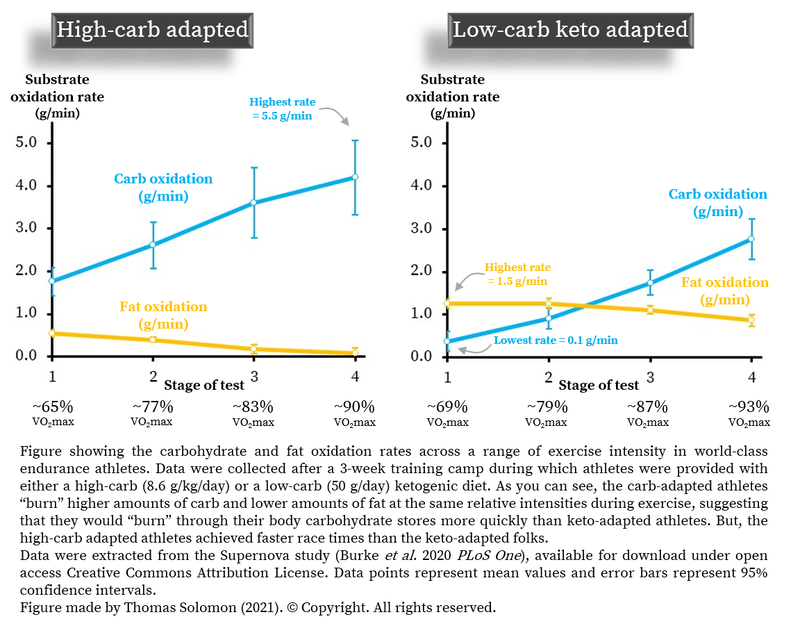
The data showed that the highest rate of fat oxidation at a low-to-moderate intensity (equivalent to an Easy run pace) was about 1.5 grams per minute and was reported in an athlete in the keto-adaptation group. It would take that athlete many moons to “burn” through their ~10 kgs of stored fat at 1.5 g/min. At “easy run pace”, some athletes in the keto-adaptation group had carbohydrate oxidation rates as low as 0.1 g/min. At that rate, it would take ~83-hours to “burn” through 500-grams of bodily glycogen stores (400 g muscle + 100 g liver). This explains why some low-carb high-fat diet-adapted folks, like Michael McKnight, are able to heroically run 100-miles with no food (albeit much slower than his best time and several hours slower than Zach Bitter’s world record time, which was actually broken by Aleksandr Sorokin while I wrote this series of posts).
On the flip side, the Supernova data showed that the highest rates of carbohydrate oxidation (approx 5.5 grams/minute) were recorded during high-intensity exercise (at around 20 km race pace) in athletes in the high-carb diet-adapted group, who also raced faster than folks in the low-carb keto-adapted group. In an athlete with a glycogen store of around 500 grams, it would take about 90-minutes to completely deplete carbohydrate stores. In the Supernova study, it took athletes between 81 and 95-minutes to complete the 20km race, meaning that many athletes would have depleted their body's carbohydrate stores to critical levels during the race.
Now let’s put this into the perspective of something epic… The Eliud Kipchoge’s official marathon world-record is 2:01:39 — approximately 20.3 kph or 2.96 mins/km. As recently documented by Andy Jones in the Journal of Applied Physiology,
 the average running economy of a world-class “Breaking2” marathon runner is ~191 millilitres of O2 per kg bodyweight per kilometre.
the average running economy of a world-class “Breaking2” marathon runner is ~191 millilitres of O2 per kg bodyweight per kilometre.
When running at marathon world-record pace, this is equivalent to
 ~65 millilitres of O2 per kg bodyweight per minute.
~65 millilitres of O2 per kg bodyweight per minute.
The average body mass of a “Breaking2” world-class marathoner is 59 kg, therefore, we can estimate that
 at world-record marathon pace, world-class male marathoners consume oxygen at a rate of 65 mL/kg/min ✕ 59 kg, i.e. ~4000 millilitres per minute, or 4 L/min.
at world-record marathon pace, world-class male marathoners consume oxygen at a rate of 65 mL/kg/min ✕ 59 kg, i.e. ~4000 millilitres per minute, or 4 L/min.
Because each litre of oxygen produces approximately 5 kcals of energy (or ~20 kilojoules),
 the rate of energy expenditure at world-record marathon pace for a male world-class marathoner is 4 L/min ✕ 5 kcal/L, i.e. ~20 kcal/min (~80 kJ/min).
Now, let’s run a thought experiment… If during a marathon, 100% of “Breaking2” marathoners' energy was coming from glucose, because 1-gram of carbohydrate (glucose) provides ~4 kcal (~16 kJ) of energy, a male world-class marathoner will be burning about 5 grams of glucose per minute and, at that rate, their total body glucose stores (i.e. ~500 grams) would last about 100-minutes at that pace. On the flip side, 1-gram of fat (fatty acids) provides ~10 kcals (~40 kJ) of energy and would, therefore, only be burnt at a rate of about 2 grams per minute at a world-record marathon pace. The “Breaking2” marathoners had a body fat percentage of ~8%, so their bodies store roughly 4700 grams of fat. So, at world-record pace, which requires energy at a rate of ~20 kcal/min (~80 kJ/min) for a world-class marathoner, if 100% of energy was coming from fatty acids, their large body fat store (4700 grams) would last for ~2300 minutes or ~39-hours! And this is where things get cryptic — Eliud Kipchoge cannot run at 20.3 kph for 39-hours; he can only sustain that rate of energy expenditure (or pace) for 2-hours.
the rate of energy expenditure at world-record marathon pace for a male world-class marathoner is 4 L/min ✕ 5 kcal/L, i.e. ~20 kcal/min (~80 kJ/min).
Now, let’s run a thought experiment… If during a marathon, 100% of “Breaking2” marathoners' energy was coming from glucose, because 1-gram of carbohydrate (glucose) provides ~4 kcal (~16 kJ) of energy, a male world-class marathoner will be burning about 5 grams of glucose per minute and, at that rate, their total body glucose stores (i.e. ~500 grams) would last about 100-minutes at that pace. On the flip side, 1-gram of fat (fatty acids) provides ~10 kcals (~40 kJ) of energy and would, therefore, only be burnt at a rate of about 2 grams per minute at a world-record marathon pace. The “Breaking2” marathoners had a body fat percentage of ~8%, so their bodies store roughly 4700 grams of fat. So, at world-record pace, which requires energy at a rate of ~20 kcal/min (~80 kJ/min) for a world-class marathoner, if 100% of energy was coming from fatty acids, their large body fat store (4700 grams) would last for ~2300 minutes or ~39-hours! And this is where things get cryptic — Eliud Kipchoge cannot run at 20.3 kph for 39-hours; he can only sustain that rate of energy expenditure (or pace) for 2-hours.
What does this mean?
That Kipchoge cannot sustain 20.3 kph for 39-hours (the amount of time his fat stores would theoretically allow) is evidence that fat is not the predominant fuel source used to produce energy when trying to move as fast as possible at a high intensity. Don’t start thinking, “yeah man, if only Kipchoge was fat-adapted to a ketogenic diet”. Don’t be that fool. A world-class marathoner who has run the fastest ever marathon is massively “fat-adapted” — that is, their maximal fat oxidation rate will be high and it will occur at a high fraction of their maximal aerobic capacity (VO2max) -- as a consequence of their long-term (5-10-years), high-volume (>160 kms/wk) training load. This tells us that other factors besides a large capacity to burn fat must determine endurance performance. This tells us that, even in the fastest marathon runner on Earth, the rate at which fatty acids can be delivered to the muscles’ mitochondria and metabolised to produce ATP is not rapid enough to fuel muscle contractions when moving fast. And this just reaffirms what we know about the bioenergetics of glucose and fatty acid metabolism (which you can read all about in my previous post at veohtu.com/fatoxidationrates):
 glucose produces ATP (chemical energy) 2- to 4-times faster than fatty acids,
glucose produces ATP (chemical energy) 2- to 4-times faster than fatty acids,
 glucose produces more ATP per litre of oxygen than fatty acids, and
glucose produces more ATP per litre of oxygen than fatty acids, and
 glucose uses less oxygen per gram to produce ATP than fatty acids.
glucose uses less oxygen per gram to produce ATP than fatty acids.
Simply put, from a bioenergetic perspective, carbohydrate is faster and more economical than fat.
But remember that your energy-producing glucose “burning” metabolic system is never “off”; it works simultaneously with your fatty acid “burning” system. If you are running at your Easy-pace, you will predominantly be “burning” fat but glucose is still being “burned,” just at a lower rate than when you are working harder. But, unlike your bucket load of fat, your pint glass of glucose won’t last forever. What this means is that, during all intensities of exercise, with time, muscle and liver glycogen will eventually get critically low and your blood glucose level will begin to fall.
By now, I hope to have helped you logically surmise that one of the keys to successful endurance performance might be to delay glycogen depletion for as long as possible. Hopefully, you have also realised that if you choose to line up on race day with a low carbohydrate availability — with low muscle and liver glycogen — you will negate all the hard work you’ve put in to get to that start line. Perhaps you are thinking, “if my carbohydrate (glucose) stores are very small and can be depleted relatively quickly, are there nutritional strategies I can use to help make them last the distance?”.
Well well, clever clogs; what an excellent question! But, the answer will have to wait until the next leg of this journey.
Until that time, keep training smart...
Why?
Because even at low to moderate intensities, like during an easy-effort run, when your muscles derive most of their energy from “burning” fatty acids, some energy still comes from “burning” a bit of glucose. Understanding this will help you conceptualise that both longer-duration races (raced at a lower fraction of your maximum aerobic capacity; VO2max) and high-intensity races (raced at a higher fraction of your VO2max, and therefore a higher speed) will eventually deplete your pint-glass of glucose despite having plenty left in your bucket load of fatty acids. Consequently, this framework will help you understand the need for performance nutrition to help you last the distance.
So, where do we start?
Well, since it is your muscles that are burning lots of fuel during exercise, let’s start with that part of the integrative physiology puzzle.
What happens to muscle glycogen during exercise?
If we take a journey in Doc’s DeLorean and head back to Boston in the 1920s, we can witness the first moment when humans realized that prolonged moderate- to high-intensity exercise depletes our glucose stores. In 1924, Sam Levine and colleagues at Harvard Medical School found that runners completing the Boston marathon had lower blood glucose levels than when they started, many with signs of hypoglycemia like dizziness, collapse, and confusion (likely caused by clinically meaningful low blood glucose). Some years later, in 1939, Erik Christensen and Ove Hansen found that cyclists took around 2 hours to ride to exhaustion at ~177 watts, at which point they had developed hypoglycemia (you will need to learn German or have your German-speaking wife help you translate this paper).These were seminal observations but they did not provide clues as to why blood glucose fell.
In 1961, Reichard and colleagues used an intravenous infusion of radioactive 14C-labelled glucose to show that blood glucose is taken up into exercising muscle and “burned” to produce energy. The work also demonstrated that the loss of glucose from the blood into muscle is compensated by an increase in glucose release from the liver. In 1967, Jonas Bergström and Eric Hultman used muscle biopsies to show that prolonged exercise decreases muscle glycogen levels. By using arterio-venous catheterisation across the liver, they also found that the liver releases glucose into the blood during exercise but that its attempt to keep providing glucose to working muscles by releasing more glucose into blood during exercise is insufficient to match the total amount of glucose “burned” during exercise. Remember, your body always makes fuel available to the working muscle.
In the 1970s, the muscle biopsy technique became widespread. In the context of running, in 1971 Dave Costill’s work showed the progressive decline in muscle glycogen over 3-days caused by daily high-intensity running (10-miles/day). And, in 1973, he further demonstrated that a 30 km race, run at ~83% VO2max, caused a 30% reduction in the muscles’ fat store (IMTG) and a 60% reduction in muscle glycogen levels.
Many studies have since studied muscle glycogen utilisation during exercise and, nowadays, we are confident that prolonged exercise eventually depletes muscle glycogen. To help minimise any doubt in this sentiment, in 2018, José Areta and Will Hopkins published a beautiful meta-analysis of all known clinical data, showing that higher exercise intensity and longer duration exercise are the biggest predictors of the rate of muscle glycogen use. Furthermore, it is now clear that a low-glycogen state has a dramatic effect on whole-body metabolism — for example, glycogen depletion reduces the capacity to “burn” glucose, which will reduce our capacity to go fast, and increases muscle protein breakdown, which may affect recovery (reviewed in detail by Andy Philp and colleagues in 2012). Plus, more recently, we have come to appreciate that the depletion of specific glycogen “compartments” that are bound to contractile proteins cause reduced force production (reviewed by Niels Ørtenblad’s lab in 2013), directly implicating low glycogen with muscle fatigue. When someone reaches exhaustion through “glycogen depletion”, total muscle glycogen levels are never zero. Instead, we now know that depletion of specific depots of “available” glycogen occurs in type 1 (“slow-twitch”) muscle fibres during long-duration endurance exercise and in type 2 (“fast-twitch”) fibres during high intensity or strength exercise (see reviews here and here).
OK. It is probably now pretty clear to you that prolonged exercise depletes muscle glycogen. The next important questions is:
What happens to liver glycogen during exercise?
In the second part of this series, you learnt that as exercise proceeds your muscles not only chip away at their glycogen stores but they also guzzle glucose from the blood. As your intensity of exercise increases, the rate of muscle glycogen breakdown also increases and your muscles take increasingly larger “gulps” of glucose from the blood. If your body did not have a contingency plan, the pint glass of glucose in your blood (which, remember, is only around 4 grams) would be drunk dry rapidly and you would quickly cease to exist. But, there is a contingency plan: your liver. It is awesome.Many moons ago, Lars Nilsson & Eric Hultman used arterio-venous catheterisation across the liver to show that, in healthy folks, the liver throws glucose into the blood at about 0.15 grams per minute to help maintain normal blood glucose levels throughout the night, providing a constant fuel source for all your organs to feed on. They showed that about ½ of the liver glucose output during the first 10-hours of an overnight fast comes from liver glycogen breakdown while the other half comes from gluconeogenesis (aka “new glucose synthesis” from metabolites like glycerol, lactate, and amino acids). Such findings have been confirmed using less-invasive nuclear magnetic resonance spectroscopy methods, but these are energy costly processes that the liver cells fuel by producing energy from circulating fatty acids in the blood.
The liver can hold about 300 mmol/L of glycogen, which based on a liver volume of about 1.8 litres is equal to around 100 grams of glycogen. This amount varies little between trained athletes and untrained folks but it is related to the amount of carbohydrate eaten in the diet. It has also been known since the 60s that, in us human folks, an overnight fast massively depletes liver glycogen stores. To put that in perspective, since your liver releases glucose at ~0.15 grams per minute and about half of that comes from liver glycogen, then after a 10-hour overnight fast your liver glycogen level will be reduced to around 50-grams. But, in the 1970s, Nilsson & Hultman found that liver glycogen is rapidly restored with carbohydrate refeeding — one of the main reasons that humans eat a morning breakfast.
During exercise, the rate at which your muscles remove glucose from the blood goes waaay up — from ~0.13 to 0.16 grams per minute at rest up to ~1 to 1.5 g/min during exercise — a 6 to 10-fold increase in the amount of glucose leaving the blood every minute. And, every drop of glucose that enters muscle during exercise is “burned” — it doesn’t form new muscle glycogen. If you remember that the blood only contains about 4 grams of glucose, this means that if you did not have a liver, it would take only a few minutes for you to stop being “sweet” and the guillotine would drop. To prevent blood glucose levels from dropping — to prevent hypoglycemia — when your tissues are feasting on the blood’s sugary goodness, the rate of glucose release from the liver into the blood must also increase to maintain blood glucose levels within a healthy range (~1 g/L, or 5 mM). In 1967, Jonas Bergström and Eric Hultman used arterio-venous catheterisation across the liver to show that the rate at which the liver releases glucose into the blood increases in proportion to exercise intensity during exercise, from ~0.1 to ~0.4 g/min in an untrained person. Since then, several studies have examined this phenomenon using arterio-venous balance methods, stable isotopes, and 13C-NMR, and it is clear that large amounts of liver-derived glucose are “burned” by muscles during exercise (see here here, here, and here). Furthermore, during long-duration (~3-hours) moderate-intensity exercise (70% VO2max), liver glucose output into the blood can reach ~1 g/min in endurance-trained athletes.
However, this increase in liver glucose output comes at a cost:
Liver glycogen.
It is tricky to study liver glycogen in humans because of the high risk of using liver biopsies during exercise. So, alternative indirect methods with stable isotope tracers or arterio-venous balance measurements of glucose-producing substrates being taken up into the liver have been used to estimate glycogen synthesis rates. Fortunately, some studies have used modern 13C-NMR methods to measure changes in liver glycogen during exercise in endurance-trained athletes. In 2000, Anna Casey et al. showed that an 80-minute ride at 70% VO2max decreased liver glycogen by about 50% from ~120 grams to ~60 grams, and in 2016, Javier Gonzalez et al. found that following 3-hours of low-intensity cycling at 50% VO2max, liver glycogen decreased by about 40% from ~140 grams to ~90 grams.
A meta-regression of all known clinical data by Javier Gonzalez clearly shows that the rate of liver glycogen depletion increases dramatically with increasing exercise intensity, but only in untrained folks. In endurance athletes, the rate of liver glycogen breakdown during exercise is lower than that of regular folks and rises to a lesser degree across a range of exercise intensities (see full table of studies here).
×
![]()
Pretty darn cool.
Yes, indeed. But there are a couple of caveats...
During exercise, the liver releases glucose into the blood and, in humans, this is predominantly from the breakdown of liver glycogen stores (rather than from gluconeogenesis of “new” glucose). Therefore, when liver glucose output is supporting moderate to high intensity exercise at a rate of 1 g/min, most of this glucose is coming from liver glycogen breakdown and, since your liver stores about 100 grams of glycogen, it will take about 100-minutes (1h40m) to completely deplete your liver glycogen store. Furthermore, let’s not forget that, during exercise, your liver tries its best to keep glucose — your economical and high-energy yielding fuel — available to the muscle. During the early stages of exercise, it is typical to see the liver release glucose into blood at a slightly higher rate than glucose is removed from blood (into muscle). Therefore, blood glucose levels often rise a little bit — there is a slight mismatch between glucose leaving and glucose entering the blood. But another mismatch occurs during prolonged exercise when liver glycogen levels become depleted. Then, the liver cannot release glucose at the rate needed to match the high rate of glucose uptake into muscle, which can be ~1 to 1.5 g/min during exercise.
The consequence?
If your liver glycogen “runs” out (pun entirely intended) and/or if your liver’s capacity to produce new glucose (via gluconeogenesis) is exceeded, blood glucose levels will begin to drop, resulting in hypoglycaemia, the signs of which are not pleasant — excess sweating, shivering, nausea, dizziness, etc. To put this in context, hypoglycaemia can arise if your race is long enough or intense enough or if your liver and muscle glycogen levels were already low to begin. When this happens, it is possible that hypoglycaemia likely acts as a “fatigue signal” to the brain — your rating of perceived exertion (RPE) goes up (exercise feels harder), your power output drops (you slow down), and you are soon forced to stop… probably because your clever brain wants to protect the beautiful body it needs so it can maintain a purpose in life. So, if your liver gets “tired” of producing glucose during exercise, your race plans will pretty quickly get eff dup. Your liver is awesome but it can only work so hard.
Note: For an excellent overview of how precious the few grams of glucose in your blood is, please read George Brooks’ 2020 narrative review. Or, for a visual representation of how this works, watch my animation below:
Hearing about glycogen depletion and hypoglycemia is all very depressing, so let’s turn our attention to something way more positive!
How long can you theoretically go?
You already know what your body stores: ~10 kilograms of fat (in a 65 kg person with 15% body fat), equivalent to ~100’000 kcals of energy, ~400 grams of muscle glycogen (~1600 kcals), ~100 grams of liver glycogen (~400 kcals), with ~4 grams of glucose (~16 kcals) circulating in the blood. These ingredients are the essence of my bucket load of fatty acids and a pint-glass of glucose analogy.You also know that as you work harder, you use relatively more glucose than fatty acids to fuel your forward progress. Because of the limited size of your bodily carbohydrate store, it is very wise to assume that you are “metabolically” limited in how long you can proceed before fatigue sets in. And, as I mentioned at the beginning of this post, this is without even considering other important contributors to fatigue like training status, hydration, body temperature, or motivation, etc.
During an Easy-effort low-to-moderate-intensity run (i.e. 60% VO2max), your body is merely “drip feeding” from its carbohydrate stores (glycogen) at a rate of ~1 gram per minute, and so it will take a few hours to deplete your glycogen stores to critical levels. On the contrary, during very high intensities (i.e. above 90% and even beyond 100% VO2max), which might include races from 800m up to 10 km, your glycogen stores are gobbled at much higher rates. But, at such high intensities, you will not deplete them to critical levels because other factors (like metabolic acidosis) will limit the duration you can work for before you reach fatigue. Where the double double toil and trouble starts to bubble is during longer duration events, where you can operate at high intensities (e.g. 70 to 90% VO2max) for durations that will deplete your glycogen stores within a couple of hours. Most folks can “squeeze” in a road half-marathon (~1 to 2-hours) before they get a visit from Macbeth’s witches but when racing for longer than around 90-minutes — 16-milers, marathons, trail races, obstacle races — glycogen depletion is a high-risk affair.
Using what you have learned so far, I will now throw you into some basic maths to help contextualize how long you can theoretically keep on rocking, from a metabolic point of view.
Let’s imagine that Bob is a well-trained club-level athlete who generally eats a moderately high carbohydrate diet, and on marathon race day — where he aims to “compete” not merely “complete” — he has eaten a carbohydrate-containing breakfast.
At his marathon pace,
and his
At marathon pace, ~80% VO2max, muscle glycogen will account for about 75% of whole-body carbohydrate “burning”. So, Bob’s.
The remaining 25% of whole-body carbohydrate “burning” will be supported by blood glucose uptake and oxidation. Therefore, his
To maintain blood glucose levels, the liver will have to match this. So, Bob’s
And, since most liver glucose output during exercise comes from glycogen, Bob’s
So, what does all this mean?
If, at the start of the race,
 Bob’s liver glycogen store was 100 grams and his muscle glycogen store was 400 grams,
Bob’s liver glycogen store was 100 grams and his muscle glycogen store was 400 grams,
at a liver glycogen breakdown rate of 1 g/min
and a simultaneous muscle glycogen breakdown rate of 3 g/min,
 Bob’s liver glycogen store would last 1-hour 40-minutes and his
Bob’s liver glycogen store would last 1-hour 40-minutes and his
 muscle glycogen store will be done after 2-hours 13-minutes.
muscle glycogen store will be done after 2-hours 13-minutes.
Therefore, because muscle and liver glycogen are simultaneously broken down during exercise, Bob’s blood glucose levels will fall around 2-hours into the race, his muscles will “feel” empty and lose power, and he won't have a hulk hand to smash through “the wall”…
Uh oh… Bob will slow down.
at a liver glycogen breakdown rate of 1 g/min
and a simultaneous muscle glycogen breakdown rate of 3 g/min,
Therefore, because muscle and liver glycogen are simultaneously broken down during exercise, Bob’s blood glucose levels will fall around 2-hours into the race, his muscles will “feel” empty and lose power, and he won't have a hulk hand to smash through “the wall”…
Uh oh… Bob will slow down.
×
![]()
How long can athletes go, in practice?
To demonstrate this framework with real observations, I “borrowed” the during-exercise substrate oxidation data from Louise Burke’s Supernova study of world-class race walkers who ate either a high-carb or a low-carb ketogenic diet for 3-weeks during a training camp. (Note: I have previously reviewed this data extensively at veohtu.com/supernova.) By compiling the post-intervention data, we can see how much fuel world-class endurance athletes burn during exercise when they are maximally “carb-adapted” (after 3-weeks of high-carb diet) or maximally “fat adapted” (after 3-weeks of a ketogenic diet).The data showed that the highest rate of fat oxidation at a low-to-moderate intensity (equivalent to an Easy run pace) was about 1.5 grams per minute and was reported in an athlete in the keto-adaptation group. It would take that athlete many moons to “burn” through their ~10 kgs of stored fat at 1.5 g/min. At “easy run pace”, some athletes in the keto-adaptation group had carbohydrate oxidation rates as low as 0.1 g/min. At that rate, it would take ~83-hours to “burn” through 500-grams of bodily glycogen stores (400 g muscle + 100 g liver). This explains why some low-carb high-fat diet-adapted folks, like Michael McKnight, are able to heroically run 100-miles with no food (albeit much slower than his best time and several hours slower than Zach Bitter’s world record time, which was actually broken by Aleksandr Sorokin while I wrote this series of posts).
On the flip side, the Supernova data showed that the highest rates of carbohydrate oxidation (approx 5.5 grams/minute) were recorded during high-intensity exercise (at around 20 km race pace) in athletes in the high-carb diet-adapted group, who also raced faster than folks in the low-carb keto-adapted group. In an athlete with a glycogen store of around 500 grams, it would take about 90-minutes to completely deplete carbohydrate stores. In the Supernova study, it took athletes between 81 and 95-minutes to complete the 20km race, meaning that many athletes would have depleted their body's carbohydrate stores to critical levels during the race.
×
![]()
To put all this in the context of running, George Brooks’ lab published a neat study examining carbohydrate dependence during marathon running, comparing fast (<2h45m) vs. slow marathoners (<3h45m). Their data confirmed that trained marathoners burn relatively more carbohydrate than fat during a marathon (in agreement with all prior data dating back to 1970: Bosch et al., Costill et al., and Adams et al.) while also showing that marathon running speed is associated with the rate of carbohydrate oxidation — faster marathoners burn more glucose.
Now let’s put this into the perspective of something epic… The Eliud Kipchoge’s official marathon world-record is 2:01:39 — approximately 20.3 kph or 2.96 mins/km. As recently documented by Andy Jones in the Journal of Applied Physiology,
When running at marathon world-record pace, this is equivalent to
The average body mass of a “Breaking2” world-class marathoner is 59 kg, therefore, we can estimate that
Because each litre of oxygen produces approximately 5 kcals of energy (or ~20 kilojoules),
What does this mean?
That Kipchoge cannot sustain 20.3 kph for 39-hours (the amount of time his fat stores would theoretically allow) is evidence that fat is not the predominant fuel source used to produce energy when trying to move as fast as possible at a high intensity. Don’t start thinking, “yeah man, if only Kipchoge was fat-adapted to a ketogenic diet”. Don’t be that fool. A world-class marathoner who has run the fastest ever marathon is massively “fat-adapted” — that is, their maximal fat oxidation rate will be high and it will occur at a high fraction of their maximal aerobic capacity (VO2max) -- as a consequence of their long-term (5-10-years), high-volume (>160 kms/wk) training load. This tells us that other factors besides a large capacity to burn fat must determine endurance performance. This tells us that, even in the fastest marathon runner on Earth, the rate at which fatty acids can be delivered to the muscles’ mitochondria and metabolised to produce ATP is not rapid enough to fuel muscle contractions when moving fast. And this just reaffirms what we know about the bioenergetics of glucose and fatty acid metabolism (which you can read all about in my previous post at veohtu.com/fatoxidationrates):
×
![]()
What can you put in your performance nutrition toolbox?
Always remember that you are the only you. Thinking about these concepts in the context of your race distance while also considering whether you plan to “compete” or simply “complete” your race distance, will help you understand the bioenergetic demands that will be placed on your body during the race. For example, during a 3000m race, you will be running at or very close to your maximal aerobic capacity (your VO2max) and will, therefore, be burning large amounts of glucose but only for ~10-minutes — your glycogen stores will not run out. During a marathon, you will be running at a lower fraction of your VO2max with less reliance on glucose as a fuel but because of the long duration, you (and even Radcliffe or Kipchoge) increase the risk of depleting your glycogen stores. This risk is high if you plan to smash your marathon; your risk is less high if you are out there to “complete” and not “compete”. In other words, if you have trained appropriately, run slow enough, and are “fat adapted” enough, you will likely make it to the finish line with no worries at all.But remember that your energy-producing glucose “burning” metabolic system is never “off”; it works simultaneously with your fatty acid “burning” system. If you are running at your Easy-pace, you will predominantly be “burning” fat but glucose is still being “burned,” just at a lower rate than when you are working harder. But, unlike your bucket load of fat, your pint glass of glucose won’t last forever. What this means is that, during all intensities of exercise, with time, muscle and liver glycogen will eventually get critically low and your blood glucose level will begin to fall.
By now, I hope to have helped you logically surmise that one of the keys to successful endurance performance might be to delay glycogen depletion for as long as possible. Hopefully, you have also realised that if you choose to line up on race day with a low carbohydrate availability — with low muscle and liver glycogen — you will negate all the hard work you’ve put in to get to that start line. Perhaps you are thinking, “if my carbohydrate (glucose) stores are very small and can be depleted relatively quickly, are there nutritional strategies I can use to help make them last the distance?”.
Well well, clever clogs; what an excellent question! But, the answer will have to wait until the next leg of this journey.
Until that time, keep training smart...
Disclaimer: I occasionally mention brands and products but it is important to know that I am not affiliated with, sponsored by, an ambassador for, or receiving advertisement royalties from any brands. I have conducted biomedical research for which I have received research money from publicly-funded national research councils and medical charities, and also from private companies, including Novo Nordisk Foundation, AstraZeneca, Amylin, A.P. Møller Foundation, and Augustinus Foundation. I’ve also consulted for Boost Treadmills and Gu Energy on their research and innovation grant applications and I’ve provided research and science writing services for Examine — some of my articles contain links to information provided by Examine but I do not receive any royalties or bonuses from those links. These companies had no control over the research design, data analysis, or publication outcomes of my work. Any recommendations I make are, and always will be, based on my own views and opinions shaped by the evidence available. My recommendations have never and will never be influenced by affiliations, sponsorships, advertisement royalties, etc. The information I provide is not medical advice. Before making any changes to your habits of daily living based on any information I provide, always ensure it is safe for you to do so and consult your doctor if you are unsure.
If you find value in this free content, please help keep it alive and buy me a beer:
 Buy me a beer.
Buy me a beer.
Share this post on your social media:
Want free exercise science education delivered to your inbox? Join the 100s of other athletes, coaches, students, scientists, & clinicians and sign up here:

About the author:
I am Thomas Solomon and I'm passionate about relaying accurate and clear scientific information to the masses to help folks meet their fitness and performance goals. I hold a BSc in Biochemistry and a PhD in Exercise Science and am an ACSM-certified Exercise Physiologist and Personal Trainer, a VDOT-certified Distance running coach, and a Registered Nutritionist. Since 2002, I have conducted biomedical research in exercise and nutrition and have taught and led university courses in exercise physiology, nutrition, biochemistry, and molecular medicine. My work is published in over 80 peer-reviewed medical journal publications and I have delivered more than 50 conference presentations & invited talks at universities and medical societies. I have coached and provided training plans for truck-loads of athletes, have competed at a high level in running, cycling, and obstacle course racing, and continue to run, ride, ski, hike, lift, and climb as much as my ageing body will allow. To stay on top of scientific developments, I consult for scientists, participate in journal clubs, peer-review papers for medical journals, and I invest every Friday in reading what new delights have spawned onto PubMed. In my spare time, I hunt for phenomenal mountain views to capture through the lens, boulder problems to solve, and for new craft beers to drink with the goal of sending my gustatory system into a hullabaloo.
Copyright © Thomas Solomon. All rights reserved.
I am Thomas Solomon and I'm passionate about relaying accurate and clear scientific information to the masses to help folks meet their fitness and performance goals. I hold a BSc in Biochemistry and a PhD in Exercise Science and am an ACSM-certified Exercise Physiologist and Personal Trainer, a VDOT-certified Distance running coach, and a Registered Nutritionist. Since 2002, I have conducted biomedical research in exercise and nutrition and have taught and led university courses in exercise physiology, nutrition, biochemistry, and molecular medicine. My work is published in over 80 peer-reviewed medical journal publications and I have delivered more than 50 conference presentations & invited talks at universities and medical societies. I have coached and provided training plans for truck-loads of athletes, have competed at a high level in running, cycling, and obstacle course racing, and continue to run, ride, ski, hike, lift, and climb as much as my ageing body will allow. To stay on top of scientific developments, I consult for scientists, participate in journal clubs, peer-review papers for medical journals, and I invest every Friday in reading what new delights have spawned onto PubMed. In my spare time, I hunt for phenomenal mountain views to capture through the lens, boulder problems to solve, and for new craft beers to drink with the goal of sending my gustatory system into a hullabaloo.
Copyright © Thomas Solomon. All rights reserved.