Education for runners and endurance athletes. Learn to train smart, run fast, and be strong.
These articles are free.
Please help keep them alive by buying me a beer:
 Buy me a beer.
Buy me a beer.
This article is part of a series:
Why has the simple act of drinking water become the most confusing topic in sports nutrition?
→ Part 1 — What we know
→ Part 2 — What we aren’t sure about
→ Part 3 — What we don’t know
→ Part 4 — What you can do
Why has the simple act of drinking water become the most confusing topic in sports nutrition?
→ Part 1 — What we know
→ Part 2 — What we aren’t sure about
→ Part 3 — What we don’t know
→ Part 4 — What you can do
“Drowning” in hydration. Part 1 of 4:
What we know about hydration and exercise — Fundamental physiology.
Thomas Solomon PhD.
15th August 2021.
The feeling of thirst, which drives your desire to drink fluid, is one of the most tightly regulated processes in the human body. So why are there so many reminders about how to stay hydrated? And, why is it all so complicated? This series will deconstruct the flood of information in four parts, addressing “what we know”, “what we aren’t sure about”, “what we don’t know”, and “what you can do”. Here, in part 1, I will bomb-dive into the pool of hydration to see what we know.
Reading time ~20-mins.
Or listen to the Podcast version.
Or listen to the Podcast version.
When Coach Klein yelled “Water sucks. It really, really sucks!” at Bobby Boucher, he was so wrong. Water is amazing. Water has flowed itself into every nook and cranny of our world, covering about three-quarters of the globe. It makes up 50 to 70% of our body weight. Water moves. Sometimes fast; sometimes slow. And, we harness its movement to produce electrical energy. Water holds boats and transports us around. It keeps us cool. It keeps us warm. It cooks our food. It keeps us alive. So, Coach Klein, water does not suck; water is life.
But you can always have too much of a good thing… Water can kill you. You can drown in it, you can boil in it, you can freeze in it. More to the point, the amount of water in your body can kill you, too little or too much. So, in these contexts, yes, “Water sucks. It really, really sucks!.
Fortunately, the amount of water in your body is so immaculately regulated that you don't really need to think about it. A bit like breathing. So, why have many folks on our watery globe lost their minds and become so keen on frequently telling us how to drink water? It must be a “first world” problem because I imagine that natives to hot and drought-prone environments probably roll their water-filled eyes at the truth that folks who live in countries with freshwater taps in every home are bombarded with guidelines on how and when to drink. Well, that is what’s flowing through my mind today and, if you’re following this, is now what flows through yours too. So…
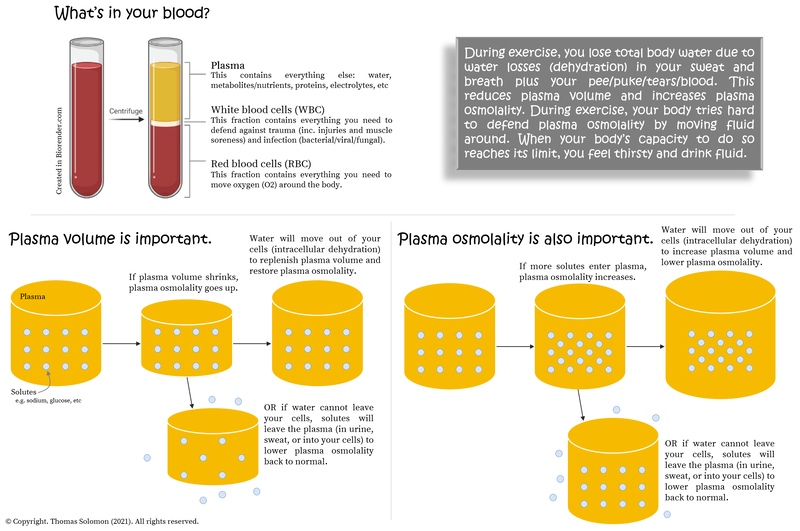
Water accounts for ~60% of your body weight (ranging from ~50 to 70% depending on your fat-free mass — more fat-free mass, more water). You can conceptualise your total body water as a “tank” from which water leaves (to remove unwanted things) and into which water flows (to replenish a low tank). But your tank of total body water is divided into an intracellular “pool” (in your cells; about ⅔ of body water) and an extracellular “pool” (interstitial fluid around your cells and plasma in your blood; about ⅓ of body water) and water constantly moves between these pools.
To maintain life, you must maintain total body water (you need to maintain euhydration). To do so, you drink fluid and eat food. Hydration is the process of adding water into your total body water, where “hypohydration” describes a lack of water entering the tank and “hyperhydration” is too much water entering the tank. On the other hand, Dehydration is the process by which water leaves your total body water — water leaves the tank in your pee, your poop, your puke, and your tears; water leaves the tank if you bleed or lactate; and, water evaporates from your skin (aka, sweat) and it leaves in your expired breath. Basically, whenever water leaves your body, dehydration occurs.
Water leaving the tank concentrates solutes in the tank. Solutes are molecules floating around in body water. Water entering the pool dilutes solutes. But, just like water, solutes also constantly move between the extracellular and intracellular pools and can enter and leave the tank. Think of this as the balance between the amount of water you add to your energy drink powder (the solute) — too much water makes the solute less concentrated/more diluted and too little water makes the solute more concentrated. The concentration of solutes in your body water determines the osmolality of the pool, which is like a “liquid pressure” that helps maintain blood (plasma) volume and cellular function. If there are more solutes like glucose, urea, and sodium dissolved in the same amount of water or if less water is dissolving the same number of solutes, the “liquid pressure” goes up.
During exercise, a disturbance in the force there is... water leaves the blood, either heading into muscle cells or leaving your body in several ways: in your breath, sweat, pee (and your tears, poop, blood, and puke, if the session or race is going poorly). As you move faster you breathe faster and, therefore, there is greater potential to lose water vapour in your breath. But, during exercise, sweat is the largest source of water removal (dehydration) from your body. Why? Because your body needs to keep cool and aims to maintain thermoneutrality at ~37oC so you can keep on rocking.
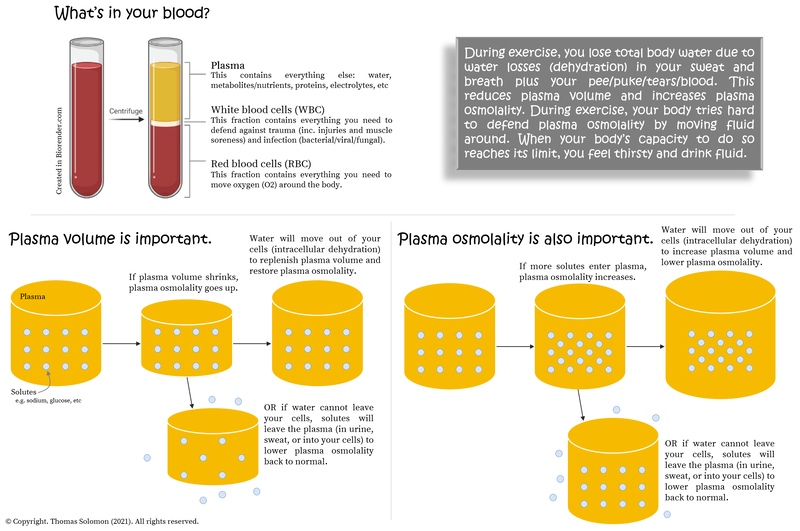
Water leaving the blood causes “hemoconcentration”, which means that plasma solutes (like sodium) become more concentrated (not less) and osmolality increases. To help maintain blood (plasma) volume and dilute solute (e.g. sodium) levels back to normal, water moves out of cells (dehydrating the intracellular pool) and into the blood (hydrating the extracellular pool) to bring osmolality back down to normal. But, of course, this means there is less water in your cells and intracellular solutes become concentrated. But, because you have been sweating, there is no water available to replenish that pool. Phew.
But it is even more complicated than water moving in and out of pools; solutes do too! Solutes like sodium and glucose, for example, also leave the blood during exercise thus decreasing plasma osmolality. To correct that, either water leaves the blood moving into cells/sweat/urine (dehydrating the extracellular pool) or solutes like sodium and glucose enter the blood to raise osmolality back up to normal. Yikes. You can probably see a circular argument evolving…
Essentially, during exercise, the large disturbance in the force causes water to leave your tank (dehydration). And, as you have probably surmised, putting water back into the tank — drinking — will help restore balance. So...
So, to summarise thus far, quite simply:
 Hydration status = Fluid in (hydration) vs. Fluid out (dehydration)
Hydration status = Fluid in (hydration) vs. Fluid out (dehydration)
Fluid in is simple; water enters the body when you drink and eat. Fluid out is more complex; water leaves the body through breathing, sweating, crying, pissing, pooping, lactating, bleeding and puking. All athletes know that exercise increases most of these things. Therefore, your sessions and races remove water from your body. But maintaining the water level in your tank (euhydration) does not mean finding strategies to sweat/breath/cry/piss/poop/lactate/bleed/puke less (well, bleeding and puking less is a worthy pursuit since they are pathological). Instead, maintaining euhydration is achieved by adding fluid back into the tank — you need to drink fluid (water; not sweat, tears, piss, poop, breast milk, blood or puke — that’s just weird).
But, how can you know when to drink?
Firstly remember that dehydration and thirst are different things: Dehydration is the physiological description (or fact) that water is leaving (or has left) your body, while thirst is the psychological thought that you’d like to drink.
Plasma osmolality (the “liquid pressure” that indicates how many solutes like glucose, urea, and sodium are in the blood) is maintained within a tight range (280 to 295 mOsm per kg H2O) to protect intracellular volume. When water leaves your cells (intracellular dehydration) to restore a rise in osmolality in the blood, osmoreceptors detect the change in plasma osmolality, which, if greater than a certain level, triggers the release of a hormone called arginine vasopressin (AVP) from the pituitary gland, which causes your kidneys to “reabsorb” water — you will pee less — while stimulating a feeling of thirst — you will seek water.
Clever.
On the other hand, if plasma volume drops (extracellular dehydration), not only do and osmoreceptors detect the corresponding change in osmolality but baroreceptors detect the change in volume, which, if greater than a specific amount, triggers the release of arginine vasopressin (you will pee less), activates the renin-angiotensin-aldosterone system (telling your kidneys to reabsorb more sodium) and your sympathetic nervous system (causing peripheral and renal vasoconstriction to make you sweat and pee less), all the while stimulating your feeling of thirst.
W’oh.
Even thirst is regulated by a complex pandemonium of signalling pathways in the central nervous system, including the renin-angiotensin, kallikrein-kinin, and serotonergic pathways. And, the trigger for thirst is driven by the rise in plasma osmolality (this 2018 systematic review shows how robust this response is). But, what is most fascinating, is that feelings of thirst are only triggered after dehydration has occurred and after your body has exhausted its dehydration prevention (aka antidiuresis) strategies by holding on to water (peeing and sweating less). This “trigger” occurs when total body water (your “tank”) decreases by ~2 to 4%, which coincidentally is roughly the weight loss threshold beyond which performance is said to diminish (more on that later). Plus, when you are thirsty and subsequently drink fluid, have you ever noticed that your feeling of thirst immediately disappears (before any water has made it into the blood)? This suggests that “sensors” (receptors) in your mouth or stomach send signals to your brain saying, “Hey, I drank some water. Chill.”.
Crikey!
But it doesn’t stop there… Have you ever felt a craving for something salty? Of course you have. Salt intake is also regulated by a complex interplay of neuroendocrine processes involving aldosterone and angiotensin II (you can go deep on this in a 2008 review by Joel Geerling &Arthur Loewy). Just as thirst is triggered by changes in plasma osmolality and/or volume, an appetite for salty things is triggered by a drop in plasma sodium (and a corresponding loss of plasma osmolality) that cannot be corrected by sodium moving out of cells and into plasma to restore osmolality…
All of these processes are going on all of the time! And, the best thing: you don’t even need to think about it. So,
And so, let the “fun” begin...
All that said, some folks need a “nudge” and daily hydration guidelines do exist — in the UK, for example, the Eat Well guide says to drink “6 to 8 cups or glasses a day” while in the US, recommendations are to drink ~1 millilitre of fluid per 1 kcal of energy expenditure. However, recommended intakes are actually “adequate intakes” based on the median value of water intakes self-reported in population-wide surveys; individual daily needs are hugely variable. For example, daily water needs for sedentary men can range from 1.2 to 2.5 litres per day, increasing to ~3.2 L/d when engaged in some daily physical activity, and even as high as 6 L/d for active folks living in hot environments or folks working hard in very hot conditions (e.g. firefighters). Even under standardized conditions, sweat rate variability between-people is huge (see here, here, and here). So, while daily hydration guidelines might be a good starting point, your hydration requirements should be refined based on your needs. And your hydration needs are influenced by your body mass, your activity level, and the ambient conditions (heat/humidity/altitude, etc), and change during illness (fever/vomiting/diarrhoea), pregnancy, and breastfeeding. Basically,
Knowing precisely how much to drink is tricky. Measuring total body water and/or plasma and urine osmolality or urine specific gravity (aka density) can provide accurate and reliable assessments of your hydration status under most conditions. But, these methods require expensive specialist equipment and expert interpretation and are not practical to implement on a daily basis, which is required because your hydration requirements change from day to day (for a deep-dive on these methods, I can recommend Samuel Cheuvront & Robert Kenefick’s 2014 review of dehydration). So, if you really desperately want a “biomarker” to inform your hydration needs, you need a simple alternative.
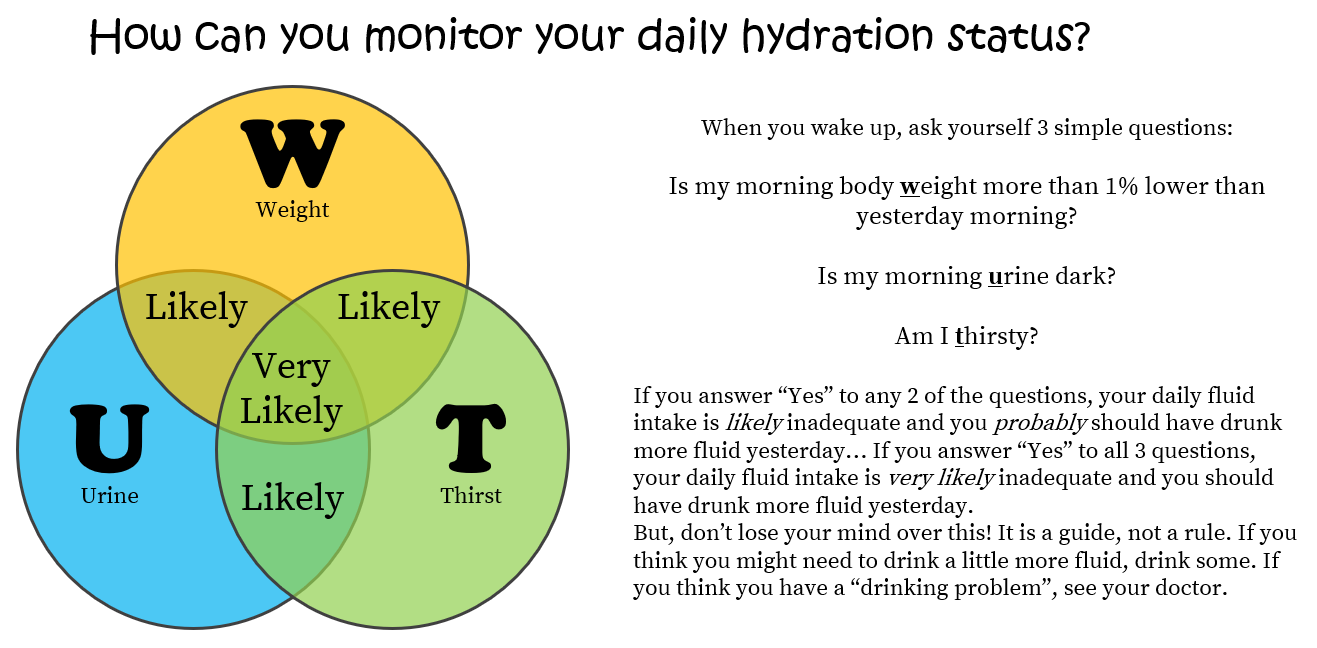
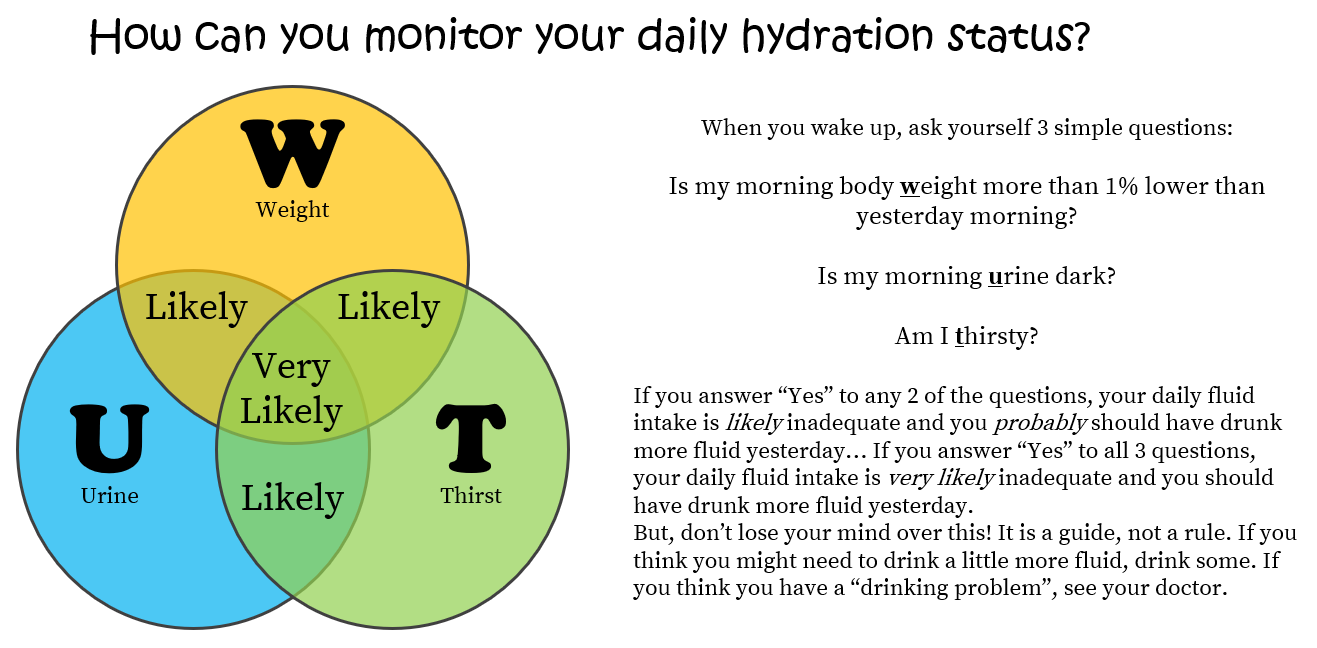
Fortunately, a simple assessment of daily hydration status has been proposed by Samuel Cheuvront and Robert Kenefick. You can do it at home — all you need is a weighing scale — and it combines 3 variables: your body Weight, Urine colour, and feeling of Thirst, measured first thing upon waking in the morning.
How does this work?
Well, your day-to-day body weight measured in no/light clothing upon waking after a toilet visit is a reasonable indicator of daily hydration status because more than 1% loss of body weight is related to increases in plasma osmolality above the threshold that triggers thirst (see here). First morning urine colour is also useful because dehydration tells the kidneys to hang on to water thus increasing the concentration of the urine — increased urine osmolality and specific gravity (density) — which is associated with dark-coloured urine (see here and here). But, don’t specifically aim for clear urine because there is no agreed consensus on whether that is useful. Furthermore, be aware that judging colour is subjective (you may use a urine colour chart to be more objective) and urine colour can be influenced by some foods in your diet. Now, because body weight and urine colour are simply biomarkers of the past 24-hours, they do not reflect immediate changes in hydration. This is where your waking thirst becomes useful since it indicates dehydration happening right here, right now (i.e. thirst responds to acute changes in hydration status).
In isolation, each marker is too unreliable — say “W U T?” — but, in concert, they have been shown to provide a useful indication of hydration status in healthy active folks, although thorough validation studies are lacking. So, your daily hydration status can easily be determined by daily tracking of your morning body Weight, Urine colour, and feeling of Thirst and, if you want to assess your daily hydration status, every morning ask yourself 3 simple questions:
 Is my morning body Weight more than 1% lower than yesterday morning? (Note that up to a 1% variation in daily body weight is normal — e.g. up to 0.6 kg if you weigh 60 kg.)
Is my morning body Weight more than 1% lower than yesterday morning? (Note that up to a 1% variation in daily body weight is normal — e.g. up to 0.6 kg if you weigh 60 kg.)
 Is my morning Urine dark?
Is my morning Urine dark?
 Am I Thirsty?
Am I Thirsty?
If you answer “Yes” to any 2 of the questions, your daily fluid intake is likely inadequate and you probably should have drunk more fluid yesterday… If you answer “Yes” to all 3 questions, your daily fluid intake is very likely inadequate and you should have drunk more fluid yesterday. But, don’t lose your mind over this… It is a guide, not a rule. If you think you might need to drink a little more fluid, drink some. If you think you have a “drinking problem”, see your doctor.
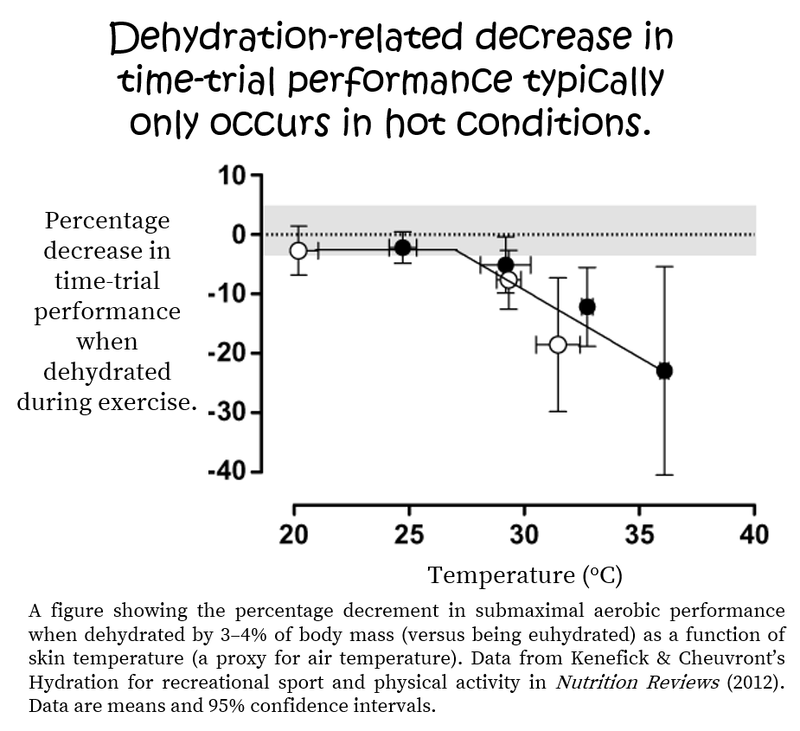
Re-used from Robert W Kenefick, Samuel N Cheuvront’s Hydration for recreational sport and physical activity. Nutrition Reviews (2012).
During my “short” 41-year presence on this Earth, there have been several iterations of during-exercise hydration guidelines — this alone has certainly helped the simple act of drinking water become the most confusing topic in sports nutrition. But, to add to the confusion, the fusion of the ubiquitous narratives of hydration guidelines from the media and social media plus the constant marketing bombardment of the latest in hydration pills and potions gives the sense that you will succumb to the serious health detriments caused by dehydration every time you exercise. This is rather alarmist. The constant warnings about “staying hydrated” must mean that dehydration-related illness during exercise is super common, right?
To help unravel this saga, the first important question to ponder is…
An observational study of 430 university/club level athletes in Ireland found that ~32% of athletes started exercise hypohydrated while a study of 17 elite soccer players in Chile found that ~47% of players were severely hypohydrated at the start of sessions and matches and only ~2% were euhydrated. To consolidate such findings, a 2019 systematic review of studies including 642 professional and recreational soccer players found that the prevalence of pre-training or pre-match hypohydration ranged from 37 to 63% (depending on how dehydration was assessed). With specific attention to running, a 2020 systematic review of trail running races, including 8644 runners, concluded that “dehydration was common among ultramarathon runners during race participation and could contribute to nausea as a common symptom”. Regrettably, however, they did not define how dehydration was assessed or provide any quantitative data. Fortunately, a thorough evaluation of ~103,000 runners over 6-years at the Comrades marathon (a 90 km road race) found that fluid and electrolyte disorders were the most common medical encounters and dehydration and muscle cramp were the most common diagnoses. But they also found that a greater risk of dehydration was associated with a higher race day temperature — if it was hot, folks were more likely to become dehydrated. On the contrary, an observational study of 83 elite marathoners and race-walkers at the very hot 2019 World Athletics Championships in Doha found that during-race dehydration was modest (average body mass loss (2.2%±1.7%); which is perhaps unsurprising in professional world-class athletes who likely have carefully-considered hydration plans for racing in the heat.
Overall, these epidemiological observations indicate that it is rather common for athletes to start exercise hypohydrated and that fluid and electrolyte-related issues do occur during exercise, especially during ultra events. However, these studies do not reveal whether this causes any pathology or performance decrement during exercise. So, the next question to ponder is…
So, although a state of dehydration before exercise and during exercise is commonly found in athletes, it is very rare that dehydration causes serious adverse health events in running, cycling, or triathlons including Ironman. In other words, stay calm and don’t turn dehydration into your biggest fear during a race. In fact, during an Ironman, your biggest water-related fear should probably be sharks.
If we are completely honest, most athletes probably don’t (but should) consider their health a priority during training and racing. So, the final question is probably something most athletes will deem most important...
It is a common cliché that a 2% loss of body mass during exercise is considered an important threshold beyond which aerobic exercise performance decreases. Sweat rate prediction models that calculate hourly and daily water needs based on metabolic rate, clothing, and environment have been used to show that, for most recreational runners, fluid losses account for less than 2% of body mass for distances up to 21 km and it is not until the marathon distance in hot conditions (30°C) that heavier individuals (80+ kg) will lose ~2% of body mass by the very end of the event (see Figure 2 here). The same prediction models show that for faster runners of all sizes, fluid losses may exceed 2% loss of body mass in both warm (22°C) and hot (30°C) conditions during a marathon but for distances up to and including 21 km, fluid losses are below 2% of body weight (see Figure 3here).
So, for slower runners looking to “complete” not “compete”, dehydration (as indicated by body weight loss) is unlikely to be an issue. For faster runners looking to “compete” on race day, bodyweight loss from fluid deficits is more likely to become an issue. But, these are prediction algorithms within which there is always a degree of error. And, never forget that you are the only you.
The notion that dehydration (indicated by body weight loss) might impair performance was born from the classic 1940s Nevada desert studies by Adolph and colleagues — when folks walked in the desert at night, the signs and symptoms of dehydration became progressively more severe after ~4–6% of body weight was lost and medical complications typically began only at bodyweight losses of 10–20%. Interestingly, the subjects chose to stop walking when they had lost about 7% of their body weight but they were able to resume walking within minutes of drinking water and most signs and symptoms of dehydration disappeared within an hour of drinking water.
While a single bodyweight measurement will tell you nothing about hydration status, changes in body weight away from your typical weight can be informative. If you are not actively trying to gain or lose body mass, your body weight will fluctuate by up to about 1% from day to day. Beyond this, it is very likely that your body water “tank” is fluctuating because, for example, an acute loss of body weight of more than 1% is related to a rise in plasma osmolality.
Consequently, over the last 80-years, there has been a lot of attention on this topic and there are currently ~3000 journal publications on (de)hydration and exercise. A 2019 narrative review, “Does Hypohydration Really Impair Endurance Performance? Methodological Considerations for Interpreting Hydration Research.”, by Lewis James and colleagues very nicely summarized what we currently know. They concluded that “hypohydration equivalent to 2–3% body mass impairs endurance exercise performance in the heat, at least when no/little fluid is ingested”. This narrative is very similar to the opinions put forward on both sides of the “Does dehydration impair exercise performance?” debate in 2007 between Michael Sawka and Tim Noakes, and is nicely illustrated in Kenefick and Cheuvront’s 2012 review of “Hydration for recreational sport and physical activity”, which highlights that dehydration impairs endurance performance only when the ambient temperature is greater than ~25°C.
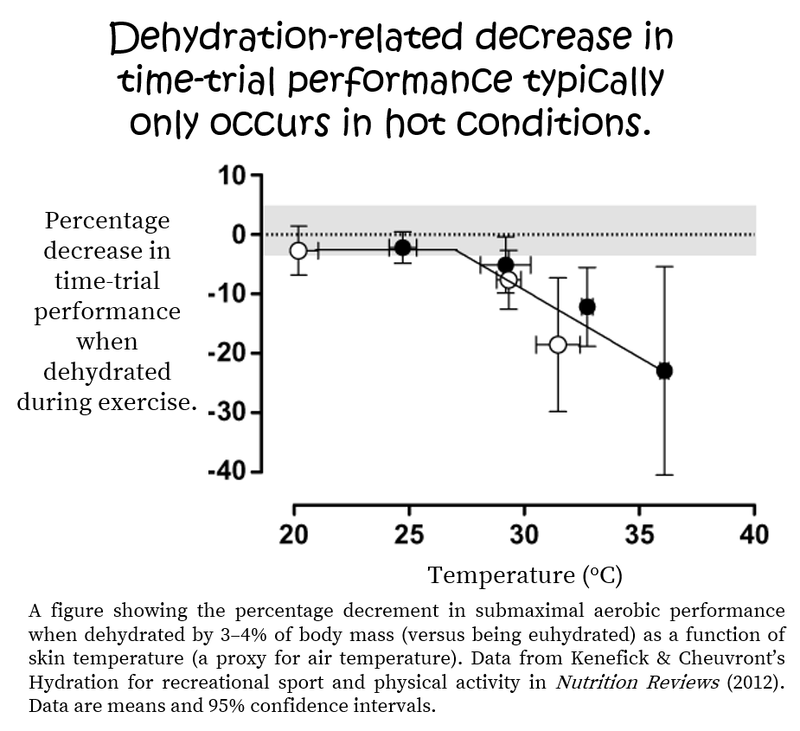
Figure from Robert W Kenefick, Samuel N Cheuvront’s Hydration for recreational sport and physical activity. Nutrition Reviews (2012).
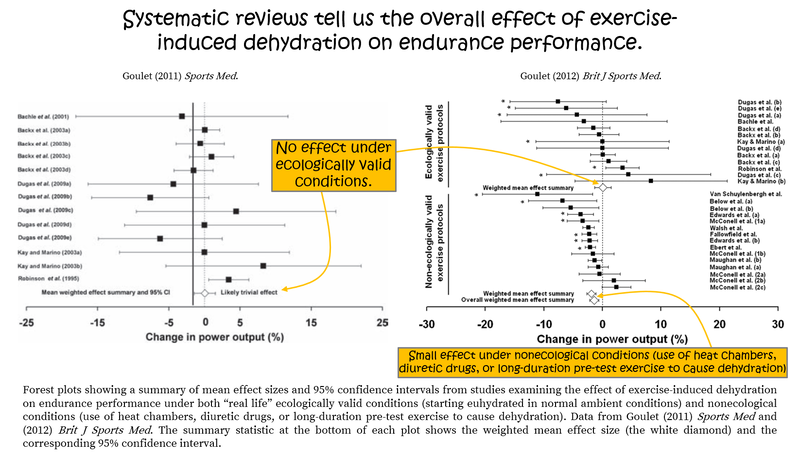
A 2019 systematic review from Deshayes and colleagues found that pre-exercise hypohydration reduces aerobic exercise performance, VO2max, and lactate threshold across a range of ambient temperatures from 19 to 40°C, emphasizing the importance of starting your sessions in a well-hydrated state. With specific attention to during-exercise dehydration, a 2011 systematic review and meta-analysis by Eric Goulet found that exercise-induced dehydration causing bodyweight loss of ≥2% impairs endurance performance, but only when combining studies using realistic (self-paced exercise) and unrealistic (fixed-power output or tests to exhaustion) exercise protocols. When only examining studies that use ecologically valid self-paced exercise protocols, exercise-induced dehydration up to 4% weight loss does not affect endurance performance under real-world conditions (when compared to maintenance of euhydration during exercise). Goulet followed up with a 2012 meta-analysis focussing on the experimental protocols used to study this topic. He concluded that that “the 2% body weight loss rule has been established from findings of studies using not ecologically valid exercise protocols and does not apply to out-of-doors exercise conditions”.
What does all this mean?
Well, while starting exercise hypohydrated is clearly not an admirable pursuit, the often quoted “rule” that 2% body weight loss during exercise impairs performance is likely an overestimate of the real effects under real conditions. This sentiment is further exemplified when looking at studies specifically examining the relationship between during-exercise weight loss and performance...
The first appealing example is that of the winner of the 2009 Dubai marathon (aka Haile Gebrselassie), who lost 9.8% (or 5.7 kg) of his body weight en route to running 2:05:29. By the power of Grayskull! But one anecdote doesn’t make a strong case. Fortunately larger observational studies exist. For example, a study of 643 marathon runners in Paris found that percentage body weight loss was associated with a faster (not slower) finishing time: Weight loss was −3.1±1.9% for runners faster than 3-hours, −2.5±2.1% for folks finishing between 3 and 4-hours, and −1.8±2.4% for runners slower than 4-hours. Similarly, a study of ~800 triathletes showed a huge range in body weight change (−10.7 to +3.7 kg) during an Ironman and, again, greater weight loss (i.e. more dehydration) was associated with a faster (not slower) finish time. And, an examination of 887 runners completing the Western State 100-miler found that weight change ranged from 8% loss to 10% gain and faster runners had lost more weight at the finish. And, finally, a very cool study of hydration status and race performance in 83 elite marathoners and race-walkers at the 2019 World Championships, showed that the extent of during-race dehydration was moderate and not correlated with either finish position or race time.
These types of observational studies trump any lab-based attempt to unravel hydration needs since they occur in the field under all the pressures and motivations needed to win a literal lump of shiny metal, which, at the world champs, indicates that you are the best in the world on that day.
What do these observations teach us?
They show us that:
 The range of body weight changes between athletes during races is enormous.
The range of body weight changes between athletes during races is enormous.
 Weight change (aka dehydration) is not predictive of finish time.
Weight change (aka dehydration) is not predictive of finish time.
 Some folks can tolerate massive dehydration and still perform highly.
Some folks can tolerate massive dehydration and still perform highly.
 Some folks drink too much fluid during exercise (hyperhydration) and gain weight, which is dangerous because it can cause hyponatremia (plasma sodium ≤135 mM).
Some folks drink too much fluid during exercise (hyperhydration) and gain weight, which is dangerous because it can cause hyponatremia (plasma sodium ≤135 mM).
So…
 In the context of a race that you start in a euhydrated state under “normal” conditions; dehydration (aka water leaving your body) during the race will probably not impair your performance.
In the context of a race that you start in a euhydrated state under “normal” conditions; dehydration (aka water leaving your body) during the race will probably not impair your performance.
 But, if it is hot and/or you start hypohydrated; then, yes, dehydration during the race will probably affect your performance.
But, if it is hot and/or you start hypohydrated; then, yes, dehydration during the race will probably affect your performance.
The ongoing, often heated, debate in this field is likely fueled by the mismatch between science and practice where in-the-lab experimental models do not truly “model” what happens on race day.
Based on what we know about human physiology and the tightly-regulated neuroendocrine control of hydration, if you are healthy, to help maintain hydration on a daily basis, it is very likely that drinking to thirst will appropriately respond to your daily needs Since our thirst mechanism evolved with us over millions of years, it is very likely that your hypothalamus knows better than any company trying to plug their latest “hydration” product. Even world-class Kenyan runners drink to thirst to maintain adequate daily hydration status. But, things can get a little more complicated during exercise and under certain conditions. There is an ongoing debate (and associated controversies, fallacies, and confusion) about how much to specifically drink during exercise — drink to thirst vs. drink to a schedule — and this is largely driven by what we don’t know… Which is exactly what I plan to drown you in next. So, stay tuned for Part 2 of this series. But, what is absolutely clear, is that starting exercise with a poor hydration status (hypohydrated or “dehydrated”) and/or not having fluid available during exercise, will amplify the effects of dehydration during exercise, which will likely impair your performance, especially on a hot day. Therefore, doing your best to stay hydrated day-to-day is an essential component of your training toolbox, and this can very likely be achieved by simply drinking some fluid when you feel thirsty.
Thanks for joining me for another “session”. Until next time, keep following your thirst.
But you can always have too much of a good thing… Water can kill you. You can drown in it, you can boil in it, you can freeze in it. More to the point, the amount of water in your body can kill you, too little or too much. So, in these contexts, yes, “Water sucks. It really, really sucks!.
Fortunately, the amount of water in your body is so immaculately regulated that you don't really need to think about it. A bit like breathing. So, why have many folks on our watery globe lost their minds and become so keen on frequently telling us how to drink water? It must be a “first world” problem because I imagine that natives to hot and drought-prone environments probably roll their water-filled eyes at the truth that folks who live in countries with freshwater taps in every home are bombarded with guidelines on how and when to drink. Well, that is what’s flowing through my mind today and, if you’re following this, is now what flows through yours too. So…
What is hydration?
Note: There are fewer clickable citations in this section because the narrative is fundamental physiology that you may read about in any human physiology textbook. If you want to go deeper, I can recommend reviews on hydration and dehydration by Drs Samuel Cheuvront & Robert Kenefick.
Water accounts for ~60% of your body weight (ranging from ~50 to 70% depending on your fat-free mass — more fat-free mass, more water). You can conceptualise your total body water as a “tank” from which water leaves (to remove unwanted things) and into which water flows (to replenish a low tank). But your tank of total body water is divided into an intracellular “pool” (in your cells; about ⅔ of body water) and an extracellular “pool” (interstitial fluid around your cells and plasma in your blood; about ⅓ of body water) and water constantly moves between these pools.
To maintain life, you must maintain total body water (you need to maintain euhydration). To do so, you drink fluid and eat food. Hydration is the process of adding water into your total body water, where “hypohydration” describes a lack of water entering the tank and “hyperhydration” is too much water entering the tank. On the other hand, Dehydration is the process by which water leaves your total body water — water leaves the tank in your pee, your poop, your puke, and your tears; water leaves the tank if you bleed or lactate; and, water evaporates from your skin (aka, sweat) and it leaves in your expired breath. Basically, whenever water leaves your body, dehydration occurs.
Water leaving the tank concentrates solutes in the tank. Solutes are molecules floating around in body water. Water entering the pool dilutes solutes. But, just like water, solutes also constantly move between the extracellular and intracellular pools and can enter and leave the tank. Think of this as the balance between the amount of water you add to your energy drink powder (the solute) — too much water makes the solute less concentrated/more diluted and too little water makes the solute more concentrated. The concentration of solutes in your body water determines the osmolality of the pool, which is like a “liquid pressure” that helps maintain blood (plasma) volume and cellular function. If there are more solutes like glucose, urea, and sodium dissolved in the same amount of water or if less water is dissolving the same number of solutes, the “liquid pressure” goes up.
During exercise, a disturbance in the force there is... water leaves the blood, either heading into muscle cells or leaving your body in several ways: in your breath, sweat, pee (and your tears, poop, blood, and puke, if the session or race is going poorly). As you move faster you breathe faster and, therefore, there is greater potential to lose water vapour in your breath. But, during exercise, sweat is the largest source of water removal (dehydration) from your body. Why? Because your body needs to keep cool and aims to maintain thermoneutrality at ~37oC so you can keep on rocking.
×
![]()
Exercise generates heat because your metabolic rate (your energy expenditure) goes up as you “burn” more fuel. Your skin cells secrete water onto the skin’s surface so your body heat can turn water from liquid to gas and carry heat into the surrounding air. Therefore, the rate of energy expenditure determines heat generation, which determines sweat rate. And… since body mass predicts energy expenditure, bigger people generate more heat. And… since a faster running speed requires a higher energy expenditure, faster runners will generate more heat. And… ambient conditions (including air temperature, humidity, and wind speed) also influence how efficiently heat leaves the body (in your sweat or breath). Therefore, the amount of water leaving the body during exercise is highly variable within and between different people.
Water leaving the blood causes “hemoconcentration”, which means that plasma solutes (like sodium) become more concentrated (not less) and osmolality increases. To help maintain blood (plasma) volume and dilute solute (e.g. sodium) levels back to normal, water moves out of cells (dehydrating the intracellular pool) and into the blood (hydrating the extracellular pool) to bring osmolality back down to normal. But, of course, this means there is less water in your cells and intracellular solutes become concentrated. But, because you have been sweating, there is no water available to replenish that pool. Phew.
But it is even more complicated than water moving in and out of pools; solutes do too! Solutes like sodium and glucose, for example, also leave the blood during exercise thus decreasing plasma osmolality. To correct that, either water leaves the blood moving into cells/sweat/urine (dehydrating the extracellular pool) or solutes like sodium and glucose enter the blood to raise osmolality back up to normal. Yikes. You can probably see a circular argument evolving…
Essentially, during exercise, the large disturbance in the force causes water to leave your tank (dehydration). And, as you have probably surmised, putting water back into the tank — drinking — will help restore balance. So...
Why do you need to hydrate?
Drinking water (during and after exercise) makes more water available to your intracellular and extracellular pools, helping to maintain or restore plasma osmolality and plasma volume. This is important because a loss of plasma volume will decrease cardiac output, causing your organs to be underperfused with blood, reducing nutrient and oxygen delivery to muscles (for ATP production) and reducing blood flow to the skin (for heat loss). Meanwhile, a loss of plasma osmolality will reduce the “liquid pressure” of your blood, which will impair the cellular entry and exit of molecules (including electrolytes and nutrients), causing organs to function suboptimally.So, to summarise thus far, quite simply:
Fluid in is simple; water enters the body when you drink and eat. Fluid out is more complex; water leaves the body through breathing, sweating, crying, pissing, pooping, lactating, bleeding and puking. All athletes know that exercise increases most of these things. Therefore, your sessions and races remove water from your body. But maintaining the water level in your tank (euhydration) does not mean finding strategies to sweat/breath/cry/piss/poop/lactate/bleed/puke less (well, bleeding and puking less is a worthy pursuit since they are pathological). Instead, maintaining euhydration is achieved by adding fluid back into the tank — you need to drink fluid (water; not sweat, tears, piss, poop, breast milk, blood or puke — that’s just weird).
But, how can you know when to drink?
Water and electrolyte balance is one of the most tightly regulated processes in the human body.
Note: Once again, there are fewer clickable citations in this section because the narrative is fundamental physiology that you may read about in any human physiology textbook or in the reviews on hydration and dehydration by Drs Samuel Cheuvront & Robert Kenefick. And, if you really want to blow your mind, I can recommend a 2019 review on Neural Control and Modulation of Thirst, Sodium Appetite, and Hunger by Augustine et al. and a 2008 review on salt appetite regulation by Joel Geerling & Arthur Loewy.
Firstly remember that dehydration and thirst are different things: Dehydration is the physiological description (or fact) that water is leaving (or has left) your body, while thirst is the psychological thought that you’d like to drink.
Plasma osmolality (the “liquid pressure” that indicates how many solutes like glucose, urea, and sodium are in the blood) is maintained within a tight range (280 to 295 mOsm per kg H2O) to protect intracellular volume. When water leaves your cells (intracellular dehydration) to restore a rise in osmolality in the blood, osmoreceptors detect the change in plasma osmolality, which, if greater than a certain level, triggers the release of a hormone called arginine vasopressin (AVP) from the pituitary gland, which causes your kidneys to “reabsorb” water — you will pee less — while stimulating a feeling of thirst — you will seek water.
Clever.
On the other hand, if plasma volume drops (extracellular dehydration), not only do and osmoreceptors detect the corresponding change in osmolality but baroreceptors detect the change in volume, which, if greater than a specific amount, triggers the release of arginine vasopressin (you will pee less), activates the renin-angiotensin-aldosterone system (telling your kidneys to reabsorb more sodium) and your sympathetic nervous system (causing peripheral and renal vasoconstriction to make you sweat and pee less), all the while stimulating your feeling of thirst.
W’oh.
Even thirst is regulated by a complex pandemonium of signalling pathways in the central nervous system, including the renin-angiotensin, kallikrein-kinin, and serotonergic pathways. And, the trigger for thirst is driven by the rise in plasma osmolality (this 2018 systematic review shows how robust this response is). But, what is most fascinating, is that feelings of thirst are only triggered after dehydration has occurred and after your body has exhausted its dehydration prevention (aka antidiuresis) strategies by holding on to water (peeing and sweating less). This “trigger” occurs when total body water (your “tank”) decreases by ~2 to 4%, which coincidentally is roughly the weight loss threshold beyond which performance is said to diminish (more on that later). Plus, when you are thirsty and subsequently drink fluid, have you ever noticed that your feeling of thirst immediately disappears (before any water has made it into the blood)? This suggests that “sensors” (receptors) in your mouth or stomach send signals to your brain saying, “Hey, I drank some water. Chill.”.
Crikey!
But it doesn’t stop there… Have you ever felt a craving for something salty? Of course you have. Salt intake is also regulated by a complex interplay of neuroendocrine processes involving aldosterone and angiotensin II (you can go deep on this in a 2008 review by Joel Geerling &Arthur Loewy). Just as thirst is triggered by changes in plasma osmolality and/or volume, an appetite for salty things is triggered by a drop in plasma sodium (and a corresponding loss of plasma osmolality) that cannot be corrected by sodium moving out of cells and into plasma to restore osmolality…
All of these processes are going on all of the time! And, the best thing: you don’t even need to think about it. So,
Why has the simple act of drinking water become the most confusing topic in sports nutrition?
 Probably because we’ve become obsessed with wanting to know how much to drink.
Probably because we’ve become obsessed with wanting to know how much to drink.
And so, let the “fun” begin...
Monitoring your daily hydration status.
The broken fire hydrant of hydration advice spurting into our lives is somewhat amusing when water and electrolyte regulation is one of the most incredibly well-regulated processes we have. When our tank is losing more water than it can hold on to, our hypothalamus tells us we feel thirsty, which indicates it is time to find fluid. The mechanisms of water and electrolyte balance that respond to dehydration and trigger thirst have been “evolutionarily conserved” in most mammals. Your ancestors got you where you are today by being epic at survival. One thing they did not need in their survival manual was an instructional section on how and when to drink water.All that said, some folks need a “nudge” and daily hydration guidelines do exist — in the UK, for example, the Eat Well guide says to drink “6 to 8 cups or glasses a day” while in the US, recommendations are to drink ~1 millilitre of fluid per 1 kcal of energy expenditure. However, recommended intakes are actually “adequate intakes” based on the median value of water intakes self-reported in population-wide surveys; individual daily needs are hugely variable. For example, daily water needs for sedentary men can range from 1.2 to 2.5 litres per day, increasing to ~3.2 L/d when engaged in some daily physical activity, and even as high as 6 L/d for active folks living in hot environments or folks working hard in very hot conditions (e.g. firefighters). Even under standardized conditions, sweat rate variability between-people is huge (see here, here, and here). So, while daily hydration guidelines might be a good starting point, your hydration requirements should be refined based on your needs. And your hydration needs are influenced by your body mass, your activity level, and the ambient conditions (heat/humidity/altitude, etc), and change during illness (fever/vomiting/diarrhoea), pregnancy, and breastfeeding. Basically,
Your hydration needs are influenced by
 anything that increases your energy expenditure
anything that increases your energy expenditure
and/or
 anything that increases your need to cool down.
anything that increases your need to cool down.
and/or
Knowing precisely how much to drink is tricky. Measuring total body water and/or plasma and urine osmolality or urine specific gravity (aka density) can provide accurate and reliable assessments of your hydration status under most conditions. But, these methods require expensive specialist equipment and expert interpretation and are not practical to implement on a daily basis, which is required because your hydration requirements change from day to day (for a deep-dive on these methods, I can recommend Samuel Cheuvront & Robert Kenefick’s 2014 review of dehydration). So, if you really desperately want a “biomarker” to inform your hydration needs, you need a simple alternative.
Fortunately, a simple assessment of daily hydration status has been proposed by Samuel Cheuvront and Robert Kenefick. You can do it at home — all you need is a weighing scale — and it combines 3 variables: your body Weight, Urine colour, and feeling of Thirst, measured first thing upon waking in the morning.
How does this work?
Well, your day-to-day body weight measured in no/light clothing upon waking after a toilet visit is a reasonable indicator of daily hydration status because more than 1% loss of body weight is related to increases in plasma osmolality above the threshold that triggers thirst (see here). First morning urine colour is also useful because dehydration tells the kidneys to hang on to water thus increasing the concentration of the urine — increased urine osmolality and specific gravity (density) — which is associated with dark-coloured urine (see here and here). But, don’t specifically aim for clear urine because there is no agreed consensus on whether that is useful. Furthermore, be aware that judging colour is subjective (you may use a urine colour chart to be more objective) and urine colour can be influenced by some foods in your diet. Now, because body weight and urine colour are simply biomarkers of the past 24-hours, they do not reflect immediate changes in hydration. This is where your waking thirst becomes useful since it indicates dehydration happening right here, right now (i.e. thirst responds to acute changes in hydration status).
In isolation, each marker is too unreliable — say “W U T?” — but, in concert, they have been shown to provide a useful indication of hydration status in healthy active folks, although thorough validation studies are lacking. So, your daily hydration status can easily be determined by daily tracking of your morning body Weight, Urine colour, and feeling of Thirst and, if you want to assess your daily hydration status, every morning ask yourself 3 simple questions:
×
![]()
But, what about monitoring your hydration status during exercise?
One thing that every clinician, scientist, coach, and athlete agrees on is that you should always aim to start a session or a race in a euhydrated state — starting dehydrated will not be fruitful nor is it safe. But how can you know how much to drink during exercise? Well… This is where the debate begins…During my “short” 41-year presence on this Earth, there have been several iterations of during-exercise hydration guidelines — this alone has certainly helped the simple act of drinking water become the most confusing topic in sports nutrition. But, to add to the confusion, the fusion of the ubiquitous narratives of hydration guidelines from the media and social media plus the constant marketing bombardment of the latest in hydration pills and potions gives the sense that you will succumb to the serious health detriments caused by dehydration every time you exercise. This is rather alarmist. The constant warnings about “staying hydrated” must mean that dehydration-related illness during exercise is super common, right?
To help unravel this saga, the first important question to ponder is…
Is clinical dehydration common in athletes?
Unfortunately, millions of people die of chronic (clinical) dehydration each year. But, this is typically due to severe acute malnutrition and/or gastrointestinal disease (e.g. cholera) and the associated vomit/diarrhoea caused by drinking contaminated water. It is sad that literally billions of people don’t have daily access to clean water while “first world” folks with their “first world” problems constantly promote “hydration” drinks to accompany their gluttonous lifestyle. But, before I get too political, stay on task, Solomon... This is about sport.An observational study of 430 university/club level athletes in Ireland found that ~32% of athletes started exercise hypohydrated while a study of 17 elite soccer players in Chile found that ~47% of players were severely hypohydrated at the start of sessions and matches and only ~2% were euhydrated. To consolidate such findings, a 2019 systematic review of studies including 642 professional and recreational soccer players found that the prevalence of pre-training or pre-match hypohydration ranged from 37 to 63% (depending on how dehydration was assessed). With specific attention to running, a 2020 systematic review of trail running races, including 8644 runners, concluded that “dehydration was common among ultramarathon runners during race participation and could contribute to nausea as a common symptom”. Regrettably, however, they did not define how dehydration was assessed or provide any quantitative data. Fortunately, a thorough evaluation of ~103,000 runners over 6-years at the Comrades marathon (a 90 km road race) found that fluid and electrolyte disorders were the most common medical encounters and dehydration and muscle cramp were the most common diagnoses. But they also found that a greater risk of dehydration was associated with a higher race day temperature — if it was hot, folks were more likely to become dehydrated. On the contrary, an observational study of 83 elite marathoners and race-walkers at the very hot 2019 World Athletics Championships in Doha found that during-race dehydration was modest (average body mass loss (2.2%±1.7%); which is perhaps unsurprising in professional world-class athletes who likely have carefully-considered hydration plans for racing in the heat.
Overall, these epidemiological observations indicate that it is rather common for athletes to start exercise hypohydrated and that fluid and electrolyte-related issues do occur during exercise, especially during ultra events. However, these studies do not reveal whether this causes any pathology or performance decrement during exercise. So, the next question to ponder is…
Are the serious adverse effects of dehydration common in athletes?
Observational data in ~800 triathletes showed a huge range in body weight loss (a biomarker for dehydration) during an Ironman race but the extent of dehydration was not associated with the prevalence of medical complications. In fact, the only athlete in the study who needed extensive medical care and hospital admission gained 3 kg during the race and was diagnosed with symptomatic hyponatremia (plasma sodium ≤135 mM) — this athlete hyperhydrated (drank too much) during the race. Furthermore, an ongoing series of studies called “Strategies to reduce Adverse medical events For the ExerciseR” (aka the SAFER study) has been documenting medical encounters during endurance running, cycling, and triathlon events. For example, over a 3-year period at the 109 km Cape Town Cycle Tour, there were 539 medical encounters among the ~100,000 race starters and the incidence rate for dehydration-related illness was 0.6 per 100,000 starters. And, in a 4-year study of ~65,000 race starters at the (21 and 56 km) Two Oceans Marathon races, there were 545 medical complications and 37 life-threatening events, of which 2 were due to significant dehydration, i.e. the incidence of dehydration-related illness was 0.18 per 100,000 starters. To help consolidate our knowledge in this area, a 2021 systematic review and meta-analysis of life-threatening and major cardiac events during marathons and ½ marathons found that over 10-years in ~1-million runners in Paris, there were 3.35 life-threatening events per 100,000 runners, mostly from major cardiac events (2.23 per 100,000, of whom a ⅓ had pre-race cardiac symptoms) and just 1.02 per 100,000 from exertional heatstroke. But among these unfortunate tragedies, there was no mention of dehydration as the cause.So, although a state of dehydration before exercise and during exercise is commonly found in athletes, it is very rare that dehydration causes serious adverse health events in running, cycling, or triathlons including Ironman. In other words, stay calm and don’t turn dehydration into your biggest fear during a race. In fact, during an Ironman, your biggest water-related fear should probably be sharks.
If we are completely honest, most athletes probably don’t (but should) consider their health a priority during training and racing. So, the final question is probably something most athletes will deem most important...
Does dehydration impair performance?
And, this is where things get even more fun...It is a common cliché that a 2% loss of body mass during exercise is considered an important threshold beyond which aerobic exercise performance decreases. Sweat rate prediction models that calculate hourly and daily water needs based on metabolic rate, clothing, and environment have been used to show that, for most recreational runners, fluid losses account for less than 2% of body mass for distances up to 21 km and it is not until the marathon distance in hot conditions (30°C) that heavier individuals (80+ kg) will lose ~2% of body mass by the very end of the event (see Figure 2 here). The same prediction models show that for faster runners of all sizes, fluid losses may exceed 2% loss of body mass in both warm (22°C) and hot (30°C) conditions during a marathon but for distances up to and including 21 km, fluid losses are below 2% of body weight (see Figure 3here).
So, for slower runners looking to “complete” not “compete”, dehydration (as indicated by body weight loss) is unlikely to be an issue. For faster runners looking to “compete” on race day, bodyweight loss from fluid deficits is more likely to become an issue. But, these are prediction algorithms within which there is always a degree of error. And, never forget that you are the only you.
The notion that dehydration (indicated by body weight loss) might impair performance was born from the classic 1940s Nevada desert studies by Adolph and colleagues — when folks walked in the desert at night, the signs and symptoms of dehydration became progressively more severe after ~4–6% of body weight was lost and medical complications typically began only at bodyweight losses of 10–20%. Interestingly, the subjects chose to stop walking when they had lost about 7% of their body weight but they were able to resume walking within minutes of drinking water and most signs and symptoms of dehydration disappeared within an hour of drinking water.
While a single bodyweight measurement will tell you nothing about hydration status, changes in body weight away from your typical weight can be informative. If you are not actively trying to gain or lose body mass, your body weight will fluctuate by up to about 1% from day to day. Beyond this, it is very likely that your body water “tank” is fluctuating because, for example, an acute loss of body weight of more than 1% is related to a rise in plasma osmolality.
Consequently, over the last 80-years, there has been a lot of attention on this topic and there are currently ~3000 journal publications on (de)hydration and exercise. A 2019 narrative review, “Does Hypohydration Really Impair Endurance Performance? Methodological Considerations for Interpreting Hydration Research.”, by Lewis James and colleagues very nicely summarized what we currently know. They concluded that “hypohydration equivalent to 2–3% body mass impairs endurance exercise performance in the heat, at least when no/little fluid is ingested”. This narrative is very similar to the opinions put forward on both sides of the “Does dehydration impair exercise performance?” debate in 2007 between Michael Sawka and Tim Noakes, and is nicely illustrated in Kenefick and Cheuvront’s 2012 review of “Hydration for recreational sport and physical activity”, which highlights that dehydration impairs endurance performance only when the ambient temperature is greater than ~25°C.
×
![]()
Narrative reviews and op-eds are fine and often provide food (or fluid) for thought but, when considering there are 3000 published papers, an objective and systematic review should be possible...
A 2019 systematic review from Deshayes and colleagues found that pre-exercise hypohydration reduces aerobic exercise performance, VO2max, and lactate threshold across a range of ambient temperatures from 19 to 40°C, emphasizing the importance of starting your sessions in a well-hydrated state. With specific attention to during-exercise dehydration, a 2011 systematic review and meta-analysis by Eric Goulet found that exercise-induced dehydration causing bodyweight loss of ≥2% impairs endurance performance, but only when combining studies using realistic (self-paced exercise) and unrealistic (fixed-power output or tests to exhaustion) exercise protocols. When only examining studies that use ecologically valid self-paced exercise protocols, exercise-induced dehydration up to 4% weight loss does not affect endurance performance under real-world conditions (when compared to maintenance of euhydration during exercise). Goulet followed up with a 2012 meta-analysis focussing on the experimental protocols used to study this topic. He concluded that that “the 2% body weight loss rule has been established from findings of studies using not ecologically valid exercise protocols and does not apply to out-of-doors exercise conditions”.
×
![]()
Besides physical performance, a 2018 meta-analysis examined the effects of dehydration (induced by exercise, heat exposure ≥27°C, exercise + heat exposure, or fluid restriction) on cognitive performance tasks (including executive function — a set of cognitive processes and mental skills that help you plan, monitor, and successfully execute your goals — reaction times, attention, and motor coordination), finding that dehydration has a small detrimental effect on cognitive performance (effect size = −0.31 to −0.11; P < 0.0001) but with large between-study variability.
What does all this mean?
Well, while starting exercise hypohydrated is clearly not an admirable pursuit, the often quoted “rule” that 2% body weight loss during exercise impairs performance is likely an overestimate of the real effects under real conditions. This sentiment is further exemplified when looking at studies specifically examining the relationship between during-exercise weight loss and performance...
The first appealing example is that of the winner of the 2009 Dubai marathon (aka Haile Gebrselassie), who lost 9.8% (or 5.7 kg) of his body weight en route to running 2:05:29. By the power of Grayskull! But one anecdote doesn’t make a strong case. Fortunately larger observational studies exist. For example, a study of 643 marathon runners in Paris found that percentage body weight loss was associated with a faster (not slower) finishing time: Weight loss was −3.1±1.9% for runners faster than 3-hours, −2.5±2.1% for folks finishing between 3 and 4-hours, and −1.8±2.4% for runners slower than 4-hours. Similarly, a study of ~800 triathletes showed a huge range in body weight change (−10.7 to +3.7 kg) during an Ironman and, again, greater weight loss (i.e. more dehydration) was associated with a faster (not slower) finish time. And, an examination of 887 runners completing the Western State 100-miler found that weight change ranged from 8% loss to 10% gain and faster runners had lost more weight at the finish. And, finally, a very cool study of hydration status and race performance in 83 elite marathoners and race-walkers at the 2019 World Championships, showed that the extent of during-race dehydration was moderate and not correlated with either finish position or race time.
These types of observational studies trump any lab-based attempt to unravel hydration needs since they occur in the field under all the pressures and motivations needed to win a literal lump of shiny metal, which, at the world champs, indicates that you are the best in the world on that day.
What do these observations teach us?
They show us that:
So, does dehydration impair performance?
The current evidence suggests that there is little need to continually debate this question. Laboratory studies clearly show that performance will likely be impaired if you start to exercise when your total body water (your tank) has been purposefully reduced (by exposure to hot conditions, prolonged exercise, diuretics, or restriction of water intake) and/or you are prevented from drinking during exercise and lose more than ~2% body weight, especially in warm/hot conditions. But, field studies show that, when starting exercise euhydrated and when allowed access to fluid during exercise, the magnitude of body weight loss (a biomarker of dehydration), even beyond 2%, is not correlated with a loss of performance (except in hot conditions). Some field studies, which included some of the best endurance athletes on Earth, even show that some athletes can tolerate as much as 10% weight loss and still perform highly!?So…
The ongoing, often heated, debate in this field is likely fueled by the mismatch between science and practice where in-the-lab experimental models do not truly “model” what happens on race day.
What can you add to your hydration toolbox?
Your total body water “tank” is tightly regulated. During prolonged exercise, your body primarily defends plasma osmolality (“liquid pressure”) not plasma volume by maintaining solute concentrations at healthy levels. To do so, water and solutes (e.g. sodium) move into and out of the intracellular and extracellular “pools”. When these mechanisms cannot maintain plasma osmolality or volume, thirst is triggered and you feel like you want to drink fluid. During exercise, your body loses water (dehydration) faster than at rest. The three main factors governing fluid loss (from sweat and breath) during exercise are your body weight, your rate of energy expenditure (e.g. running speed), and the ambient conditions (including air temperature, humidity, and wind speed). Therefore, sweat rates are highly variable within and between different people.Based on what we know about human physiology and the tightly-regulated neuroendocrine control of hydration, if you are healthy, to help maintain hydration on a daily basis, it is very likely that drinking to thirst will appropriately respond to your daily needs Since our thirst mechanism evolved with us over millions of years, it is very likely that your hypothalamus knows better than any company trying to plug their latest “hydration” product. Even world-class Kenyan runners drink to thirst to maintain adequate daily hydration status. But, things can get a little more complicated during exercise and under certain conditions. There is an ongoing debate (and associated controversies, fallacies, and confusion) about how much to specifically drink during exercise — drink to thirst vs. drink to a schedule — and this is largely driven by what we don’t know… Which is exactly what I plan to drown you in next. So, stay tuned for Part 2 of this series. But, what is absolutely clear, is that starting exercise with a poor hydration status (hypohydrated or “dehydrated”) and/or not having fluid available during exercise, will amplify the effects of dehydration during exercise, which will likely impair your performance, especially on a hot day. Therefore, doing your best to stay hydrated day-to-day is an essential component of your training toolbox, and this can very likely be achieved by simply drinking some fluid when you feel thirsty.
Thanks for joining me for another “session”. Until next time, keep following your thirst.
Disclaimer: I occasionally mention brands and products but it is important to know that I am not affiliated with, sponsored by, an ambassador for, or receiving advertisement royalties from any brands. I have conducted biomedical research for which I have received research money from publicly-funded national research councils and medical charities, and also from private companies, including Novo Nordisk Foundation, AstraZeneca, Amylin, A.P. Møller Foundation, and Augustinus Foundation. I’ve also consulted for Boost Treadmills and Gu Energy on their research and innovation grant applications and I’ve provided research and science writing services for Examine — some of my articles contain links to information provided by Examine but I do not receive any royalties or bonuses from those links. These companies had no control over the research design, data analysis, or publication outcomes of my work. Any recommendations I make are, and always will be, based on my own views and opinions shaped by the evidence available. My recommendations have never and will never be influenced by affiliations, sponsorships, advertisement royalties, etc. The information I provide is not medical advice. Before making any changes to your habits of daily living based on any information I provide, always ensure it is safe for you to do so and consult your doctor if you are unsure.
If you find value in this free content, please help keep it alive and buy me a beer:
 Buy me a beer.
Buy me a beer.
Share this post on your social media:
Want free exercise science education delivered to your inbox? Join the 100s of other athletes, coaches, students, scientists, & clinicians and sign up here:

About the author:
I am Thomas Solomon and I'm passionate about relaying accurate and clear scientific information to the masses to help folks meet their fitness and performance goals. I hold a BSc in Biochemistry and a PhD in Exercise Science and am an ACSM-certified Exercise Physiologist and Personal Trainer, a VDOT-certified Distance running coach, and a Registered Nutritionist. Since 2002, I have conducted biomedical research in exercise and nutrition and have taught and led university courses in exercise physiology, nutrition, biochemistry, and molecular medicine. My work is published in over 80 peer-reviewed medical journal publications and I have delivered more than 50 conference presentations & invited talks at universities and medical societies. I have coached and provided training plans for truck-loads of athletes, have competed at a high level in running, cycling, and obstacle course racing, and continue to run, ride, ski, hike, lift, and climb as much as my ageing body will allow. To stay on top of scientific developments, I consult for scientists, participate in journal clubs, peer-review papers for medical journals, and I invest every Friday in reading what new delights have spawned onto PubMed. In my spare time, I hunt for phenomenal mountain views to capture through the lens, boulder problems to solve, and for new craft beers to drink with the goal of sending my gustatory system into a hullabaloo.
Copyright © Thomas Solomon. All rights reserved.
I am Thomas Solomon and I'm passionate about relaying accurate and clear scientific information to the masses to help folks meet their fitness and performance goals. I hold a BSc in Biochemistry and a PhD in Exercise Science and am an ACSM-certified Exercise Physiologist and Personal Trainer, a VDOT-certified Distance running coach, and a Registered Nutritionist. Since 2002, I have conducted biomedical research in exercise and nutrition and have taught and led university courses in exercise physiology, nutrition, biochemistry, and molecular medicine. My work is published in over 80 peer-reviewed medical journal publications and I have delivered more than 50 conference presentations & invited talks at universities and medical societies. I have coached and provided training plans for truck-loads of athletes, have competed at a high level in running, cycling, and obstacle course racing, and continue to run, ride, ski, hike, lift, and climb as much as my ageing body will allow. To stay on top of scientific developments, I consult for scientists, participate in journal clubs, peer-review papers for medical journals, and I invest every Friday in reading what new delights have spawned onto PubMed. In my spare time, I hunt for phenomenal mountain views to capture through the lens, boulder problems to solve, and for new craft beers to drink with the goal of sending my gustatory system into a hullabaloo.
Copyright © Thomas Solomon. All rights reserved.